Back to Journals » International Journal of Nanomedicine » Volume 19
Advances in Engineered Nanoparticles for the Treatment of Ischemic Stroke by Enhancing Angiogenesis
Authors Wang G, Li Z, Wang G, Sun Q, Lin P, Wang Q, Zhang H, Wang Y, Zhang T, Cui F, Zhong Z
Received 7 February 2024
Accepted for publication 2 May 2024
Published 17 May 2024 Volume 2024:19 Pages 4377—4409
DOI https://doi.org/10.2147/IJN.S463333
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 6
Editor who approved publication: Professor Eng San Thian
Guangtian Wang,1,2,* Zhihui Li,3,* Gongchen Wang,4,* Qixu Sun,5 Peng Lin,1 Qian Wang,2 Huishu Zhang,6 Yanyan Wang,7 Tongshuai Zhang,8 Feiyun Cui,9 Zhaohua Zhong1,2
1Teaching Center of Pathogenic Biology, School of Basic Medical Sciences, Harbin Medical University, Harbin, Heilongjiang, 150081, People’s Republic of China; 2Department of Microbiology, School of Basic Medical Sciences, Harbin Medical University, Harbin, Heilongjiang, 150081, People’s Republic of China; 3Department of Neurology, The Fourth Affiliated Hospital of Harbin Medical University, Harbin, Heilongjiang, 150086, People’s Republic of China; 4Department of Vascular Surgery, The Fourth Affiliated Hospital of Harbin Medical University, Harbin, Heilongjiang, 150086, People’s Republic of China; 5Department of Gastroenterology, Penglai People’s Hospital, Yantai, Shandong, 265600, People’s Republic of China; 6Teaching Center of Biotechnology, School of Basic Medical Sciences, Harbin Medical University, Harbin, Heilongjiang, 150081, People’s Republic of China; 7Teaching Center of Morphology, School of Basic Medical Sciences, Harbin Medical University, Harbin, Heilongjiang, 150081, People’s Republic of China; 8Department of Neurobiology, School of Basic Medical Sciences, Harbin Medical University, Harbin, Heilongjiang, 150081, People’s Republic of China; 9Department of Physiology, School of Basic Medical Sciences, Harbin Medical University, Harbin, Heilongjiang, 150081, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhaohua Zhong; Feiyun Cui, Email [email protected]; [email protected]
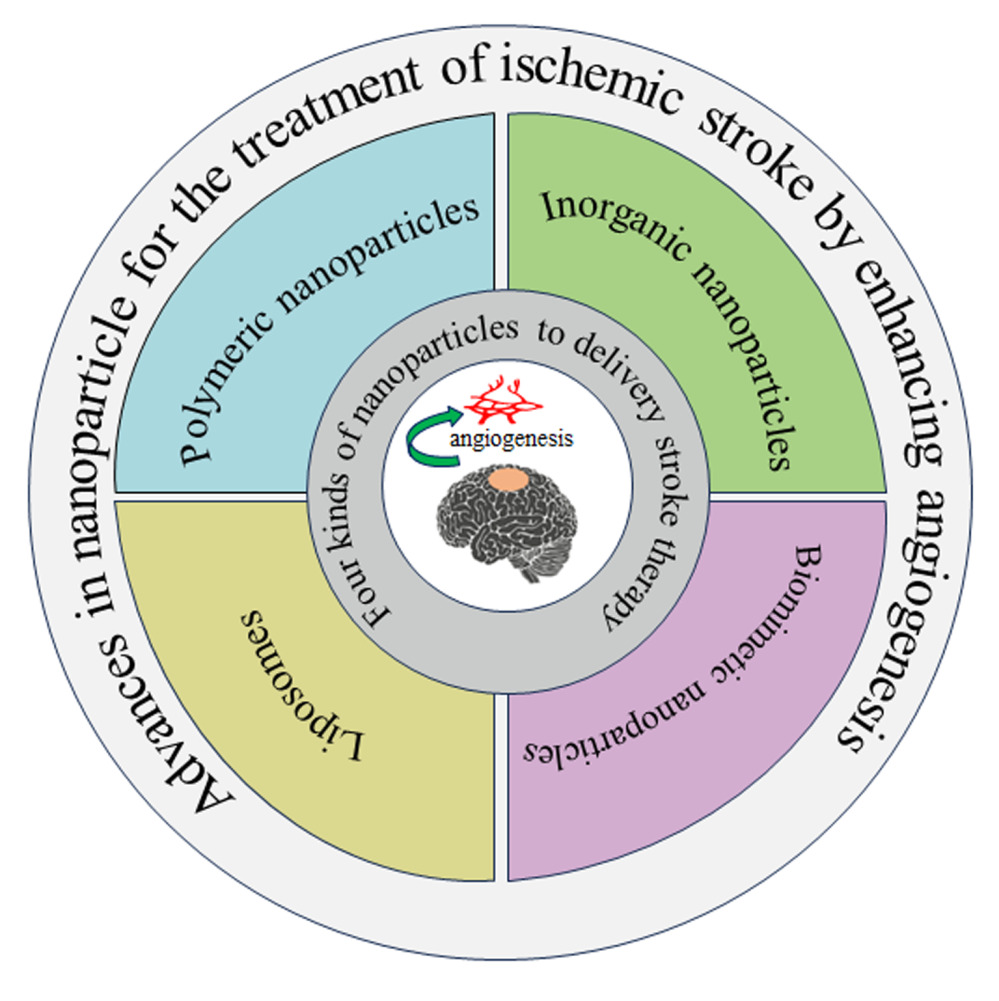
Abstract: Angiogenesis, or the formation of new blood vessels, is a natural defensive mechanism that aids in the restoration of oxygen and nutrition delivery to injured brain tissue after an ischemic stroke. Angiogenesis, by increasing vessel development, may maintain brain perfusion, enabling neuronal survival, brain plasticity, and neurologic recovery. Induction of angiogenesis and the formation of new vessels aid in neurorepair processes such as neurogenesis and synaptogenesis. Advanced nano drug delivery systems hold promise for treatment stroke by facilitating efficient transportation across the the blood-brain barrier and maintaining optimal drug concentrations. Nanoparticle has recently been shown to greatly boost angiogenesis and decrease vascular permeability, as well as improve neuroplasticity and neurological recovery after ischemic stroke. We describe current breakthroughs in the development of nanoparticle-based treatments for better angiogenesis therapy for ischemic stroke employing polymeric nanoparticles, liposomes, inorganic nanoparticles, and biomimetic nanoparticles in this study. We outline new nanoparticles in detail, review the hurdles and strategies for conveying nanoparticle to lesions, and demonstrate the most recent advances in nanoparticle in angiogenesis for stroke treatment.
Keywords: angiogenesis, ischemic stroke, nanoparticles, blood brain barrier, neurogenesis, neuroprotection therapy
Graphical Abstract:
Introduction
Ischemic stroke is a neurological condition caused by cerebrovascular stenosis or occlusion. It is the world’s second-greatest cause of mortality and the major cause of long-term impairment in people.1,2 Furthermore, as the world population ages, the prevalence of ischemic stroke rises.3 Ischemia causes the irreversible creation of a damaged infarct core and the surrounding viable penumbra in the ischemic hemisphere. Early recanalization of occluded cerebral arteries by intravenous thrombolysis or mechanical thrombectomy to decrease infarcts while salvaging the penumbra is the gold standard of therapy. Unfortunately, the clinical treatment of ischemic stroke has several limitations and requires further development owing to the restricted temporal window of intravenous thrombolysis (within 3–4.5 h after start) and the absence of universal standardization of mechanical thrombectomy procedures.4,5 Although thrombolytic therapy is strictly time-limited, timely thrombolysis can be effective in relieving neurological damage.6 The recombinant fibrinogen activator tPA is the only effective thrombolytic agent approved by the US Food and Drug Administration (FDA) for clinical use in acute ischemic stroke.7 With the development of new thrombolytic agents and advanced imaging techniques that enable longer thrombolysis times based on advanced imaging, the treatment time window has been extended to 6 h due to the short therapeutic window suitable for the majority of patients (≤4.5 h). t-PA is the only medication that is specifically indicated for the management of ischemic stroke. As a result, it is critical to develop pharmaceuticals that effectively address the requirements, facilitate appropriate treatment, and exhibit minimal to negligible adverse effects and robust potency. However, there are numerous pharmaceuticals that have the potential to slow down the pathological progression of ischemic stroke, and researchers are still exploring these to find an effective delivery system or method for cerebral transportation.
According to research, the ischemic border zone, also known as the ischemic penumbra, stays at 25–50% of preocclusion perfusion values for 6 h to several days following an acute cerebral infarction.8 Although the neuronal tissue in the ischemic penumbra is at risk, it has not yet perished. Previous research suggested that neurons might survive in the penumbra for days or weeks. Increased blood flow in the ischemic penumbra at the right moment may repair tissue damage and avoid neurological impairments.9,10 Furthermore, interventions to promote stroke recovery are critical in order to optimize patients’ functional independence and quality of life. Neurogenesis and angiogenesis are two neurorestorative activities. Angiogenesis is a fundamental characteristic of ischemic stroke recovery and neuronal post-stroke reorganization, according to emerging findings.11–14 Induction of angiogenesis and the formation of new vessels aid in neurorepair processes such as neurogenesis and synaptogenesis.14 Ischemic stroke is characterized by a sequence of alterations and vascular remodeling processes in the affected brain regions. Vascular regeneration is an essential component of ischemic disease management because it promotes the development of fresh capillaries from existing blood vessels.15 Angiogenesis, the multi-step, and highly regulated process by which new blood vessels are formed, is essential for the development, repair, and proliferation of tissues.16–18 Under normal physiological conditions, a complex interplay of proangiogenic and antiangiogenic factors closely regulates angiogenesis. This process is significantly influenced by a multitude of growth factors that aid in the preservation of capillary stability.19 The complex equilibrium between facilitating the expansion of nascent blood vessels and maintaining the integrity of the preexisting vasculature is regulated by these factors.20 These factors, in conjunction with additional pro-angiogenic cytokines, are present in the circulation in a delicate equilibrium. However, the presence of tissue hypoxia can disrupt this homeostatic equilibrium, leading to the promotion of angiogenesis and the upregulation of proangiogenic factor synthesis.21 Given the intrinsic sluggishness of the spontaneous vascular regeneration response, it is imperative to investigate potential approaches that can accelerate this phenomenon. Interestingly, the coordinated actions of numerous angiogenic factors, rather than a single factor, influence the development of fresh blood vessels. To facilitate optimal angiogenesis, we must precisely coordinate pro-angiogenic factors spatiotemporally.22,23
Although certain mechanisms are efficient in controlling angiogenesis, medication delivery remains a barrier.24 Because the BBB prevents most medications from accessing the brain, many agents must be delivered invasively. Even though BBB integrity may be reduced after ischemia shocks, the level of impairment to BBB integrity is often insufficient to fulfill appropriate drug enrichment for therapy.25 Furthermore, since many peptides and small-molecule medicines breakdown and are eliminated quickly during circulation, pharmacologically adequate concentrations and long-lasting effects cannot be ensured.8 Since well-designed nanoparticles offer several distinct benefits, many nanoparticles have been created to enhance the effectiveness and lessen the adverse effects of existing stroke therapy approaches. Furthermore, nanoparticles provide up new avenues for certain developing therapies, such as gene therapy, which is beneficial in the recovery from injury-stroke. Liposomes, polymeric nanoparticles, emerging cell membrane coated nanoparticles, and biomimetic nanoparticles are examples of nanoparticles that have been used in preclinical research to treat ischemic stroke (Figure 1). This study focuses primarily on recent breakthroughs in nanoparticle for the treatment of ischemic stroke via angiogenesis. On this premise, we expect to unveil the potentials and problems of nanoparticle in the area of ischemic stroke through angiogenesis, as well as present new ideas and perspectives for the creation of nanoparticles targeting cerebral ischemia regions for successful ischemic stroke therapy.
There are various difficulties in treating an ischemic stroke. Most treatments have a short blood circulation and are unable to efficiently pass the BBB to reach ischemic areas.26 Other intrinsic properties of nanoparticles that distinguish them from conventional medicines include the ability to modify physicochemical properties such as particle size, shape, surface charge, and hydrophobic index, which can significantly influence their internalization into the targeted cells or tissues.27 Furthermore, nanovehicle surfaces may be functionalized with different kinds of targeting ligands to define their targetability to target tissues, such as biodistribution to cerebral ischemia areas.28 Another achievement in nanoparticle design is the creation of stimuli-responsive nanocarriers that can modulate medication release inside particular ischemic tissues for stroke treatment with little off-target drug accumulation. Thus, nanoparticles are effective carriers for delivering treatments (drugs) and controlling their release in a variety of diseases.29–31 The existing hurdles in the treatment of ischemic stroke may be solved by nanoparticle-based medication delivery systems. As a result, a diverse spectrum of nanocarriers with varying sizes, surface features, and biopharmaceutical properties have been created utilizing various organic and inorganic polymers. To the best of our knowledge, numerous kinds of nanocarriers used for cerebral stroke therapy include polymeric nanoparticles, liposomes, inorganic nanoparticles, and biomimetic nanoparticles (Table 1). This review discusses several kinds of nanoparticles for the treatment of cerebral stroke through angiogenesis.
 |
Table 1 Summary of Nanoparticles for Stroke Treatment by Angiogenesis |
Polymeric Nanoparticles
Polymeric nanoparticles have been widely used in a variety of applications due to their outstanding properties, such as colloidal ranged size (1–500 nm),48 biodegradability, biocompatibility, controlled release characteristics,49–51 high encapsulation efficiency, prevention of premature degradation of labile drugs via encapsulation into polymeric matrix, efficient permeability across biological barriers, and flexibility of functionalization of surface.52 The characteristics of polymeric nanoparticles are determined by the nature/type of polymer used for engineering. Because they are nontoxic and biocompatible, as well as having a sustained-release property, biodegradable polymeric nanoparticles have been created as drug delivery carriers to treat neurological illnesses.53
Microvessels were hypoxic after an acute cerebral infarction, and apoptosis or necrosis ensued. Revascularization of blood arteries and restoration of blood flow in ischemic brain tissue may ameliorate the hypoxic status of the tissue. Neuron-protective and neurogenesis functions might be used to minimize cerebral vascular degeneration and increase microvessel formation. Ginsenoside Rg1 (Rg1) is a significant component of Panax notoginseng saponins.54 Many clinical reports and studies have shown that Rg1 has a therapy role for various central nervous system disorders such as anti-fatigue, anti-stress, anti-oxidation, anti-oedema, and the decrease of cerebral infarct volume.55 Rg1 decreased free radical damage to nerve cells, promoted nerve function reconstruction, improved angiogenesis function, increased blood flow to injured brain tissue, activated the neurotropic factor, and promoted nerve function recovery.56,57 One of the major reasons was that Rg1 could not effectively permeate the BBB and accumulate in brain regions. The BBB enabled just a few molecules to get through, limiting Rg1 ability to boost neuroprotection function in the cerebral ischemia region.55,58 The high expression of transferrin receptor (TfR) in cerebral cortex microvessels may help the nanoparticles traverse the BBB by endocytosis.59,60 c-Poly glutamic acid (PGA), the optimal drug carrier, was created by biological fermentation and was safe, nontoxic, degradable, and immunogenic. High drug wrapping rates and negligible side effects are achieved using PGA-based nano-drug carriers.61–63 Shen and colleagues employed a maleimide-fixed chitosan-c-PGA complex to self-assemble the majority of Rg1 for cerebral infarction therapy. The researchers created a PGA-TfR-targeting nanocarrier (PATRC) that can traverse the BBB and cure cerebral infarction. A TfR-targeted peptide was coupled with the hydrophobic nanocarrier wrapping Rg1.32 PATRC used cell targeting on rat brain microvascular endothelial cells RBE4 in vitro, which was identified using immunofluorescence and flow cytometry techniques. When compared to the Rg1-threatened group, the PATRC demonstrated superior tube-forming capacity in vitro. Compared to the group that was given Rg1, PATRC was able to get through the BBB in vivo, as measured by HPLC. It also decreased the size of the brain injury, as measured by TTC staining, and boosted microvascular regeneration in the injury area, as measured by CD31 immunofluorescence. TfR-mediated endocytosis by PATRC increased capillary development in the cerebral infarction site in vivo.32
An appealing therapeutic approach to promoting angiogenesis following an ischemic event is the delivery of pro-angiogenic proteins. To obtain effective and non-invasive local angiogenic therapies, a number of methods are being researched.64 Encapsulating pro-angiogenic proteins into appropriate polymeric micro-65,66 or nano-carriers67,68 is one of the most popular methods because it may retain protein structure and enable local distribution with minimal off-target effects. One of the most researched pro-angiogenic growth factors is recombinant human vascular endothelial growth factor-165 (VEGF165), which has been successfully encapsulated into poly (D,L-lactic-co-glycolic acid) (PLGA) microspheres and nanocapsules.15,66,67 In vivo studies indicate tissue revascularization and recovery in animal models of hind-limb ischemia, indicating that VEGF165 administration through PLGA carriers induces angiogenesis.69–71 The utilization of magnetic materials to aid in the on-site delivery of medicinal medicines with an external magnetic field has piqued the curiosity of many researchers. Several studies have been conducted on the encapsulation of superparamagnetic iron oxide nanoparticles (SPIONS) into PLGA particles together with pharmaceuticals for targeted drug administration and non-invasive imaging of tissues (through magnetic resonance imaging, MRI).72,73 Researchers created PLGA nanocapsules with human recombinant VEGF165 in their inner particle core and SPIONS implanted in their polymeric coating using a double-emulsion-solvent-evaporation approach.33 The nanocapsules were spherical and extremely monodisperse, with a hydrodynamic diameter of roughly 220 nm and excellent encapsulation efficiencies of both VEGF165 and SPIONS. Importantly, co-encapsulation of VEGF165 and SPIONS in the same formulation (PLGA nanocapsule) demonstrated magnetically retained protein release over time and in vitro pro-angiogenic activity by inducing human microvascular brain endothelial cell proliferation.33
Hypoxia-inducible factor 1-α (HIF-1α) is a crucial component of the transcription factor HIF-1 and functions as a sensor for hypoxia. It governs the transcriptional activity of HIF-1 and plays a critical role in regulating angiogenesis in the context of cerebral ischemia.74,75 In previous research, an HIF-1α mutant variant (referred to as HIF-1α-AA) was documented to exhibit enhanced stability. This mutant form was subsequently introduced into mesenchymal stem cells, resulting in the manifestation of neuroprotective properties against ischemic stroke.76 Researchers have shown considerable interest in the safety of nonviral gene vectors. Polymeric nanoparticles, including synthetic hyperbranched cationic polymers, have gained significant popularity as nanocarriers for the treatment of neurological disorders due to their ability to effectively transport diverse therapeutic compounds across the BBB.77 Deng et al developed a novel nonviral gene vector, specifically a hyperbranched cationic amylopectin derivative conjugated with 3-(dimethylamino) −1-propylamine (DMAPA-Amyp) nanocarrier, to encapsulate the HIF-1α-AA plasmid DNA. Furthermore, a targeting technique was implemented to specifically choose RGD peptides that would attach to the engineered nanocarrier (RGD-DMAPA-Amyp) with the purpose of targeting endothelial cells. With the help of a targeting method, nanocarriers can be sent directly to the vascular endothelial cells in the peri-infarct area of the brain. They place significant emphasis on the targeting capability of the nanocarrier and its therapeutic efficacy in the context of cerebral ischemia. The findings of the study indicate that RGD-DMAPA-Amyp exhibits favorable biocompatibility and a notable rate of cellular uptake. These results suggest that RGD-DMAPA-Amyp possesses the characteristics of a stable nonviral gene vector capable of being internalized by human cells. In the context of rat models of stroke caused by ischemic events, it was observed that the group treated with RGD-DMAPA-Amyp nanoparticles had a higher degree of aggregation in vascular endothelial cells inside the peri-infarct area as compared to the group treated with non-targeted nanocarriers. Furthermore, this targeted nanoparticle treatment led to a considerable enhancement in the recovery of neurological functions. The data suggests that the nanomedicine treated with RGD has enhanced efficacy in promoting the restoration of nerve function. Additional investigation into the mechanism of RGD-DMAPA-Amyp/HIF-1α-AA in the management of cerebral ischemia has demonstrated promising results in enhancing angiogenesis in vivo.34
The independent silencing of Hif-prolyl hydroxylase 2 (PHD2) was shown to effectively stabilise HIF-1a under normoxic conditions.78–80 The suppression of PHD2 may potentially augment the viability of endothelial progenitor cells (EPCs) in an ischemia setting through a route that is reliant on hypoxia-inducible factor 1-alpha (HIF-1α). Despite the considerable research attention devoted to siRNA therapy in many pathological conditions, several barriers have been identified that hinder the widespread implementation of siRNA. These barriers encompass the quick enzymatic degradation of siRNA and its limited cellular absorption.81 In order to address these constraints, it is imperative to devise efficacious siRNA delivery platforms capable of proficiently transporting siRNA molecules into specific cellular targets.82
Several recent studies have documented a range of vectors that may effectively transport siRNA molecules into cells. Notably, magnetic nanoparticles have emerged as particularly potent vectors due to their ability to both facilitate siRNA administration and enable imaging of the process.82 In prior studies, researchers successfully developed amphiphilic low molecular weight polyethylenimine (Alkyl-PEI) encapsulated superparamagnetic iron oxide nanoparticles (SPIONS) (Alkyl-PEI/SPIO) for the purpose of delivering siRNA and facilitating imaging.83,84 In their study, Wang et al conducted optimisation of nanoparticle-mediated siRNA administration to enhance its efficacy in EPCs. Furthermore, they successfully integrated the delivery of siRNA with the tracking of EPCs in vivo using Alkyl-SPIO/siPHD2 nanoparticles.35 The researchers effectively devised a robust siRNA delivery method that integrates siRNA delivery and the tracking of EPCs using MRI. In addition, in order to address the limitations of MRI and BLI, the researchers employed a combined approach, integrating MRI with BLI. This novel combination allowed for the non-invasive and sequential assessment of the homing/migration and survival of EPCs over a period of time. In addition, the researchers showcased that the inhibition of PHD2 resulted in a notable improvement in the effectiveness of EPCs as a therapeutic intervention for ischemic stroke. This enhancement was attributed to the heightened migratory and survival capabilities of the EPCs. The researchers provided evidence that mice treated with siPHD2-EPCs exhibited a notable decrease in infarct volume, along with enhanced angiogenesis, neurogenesis, white matter repair, and functional recovery following ischemic stroke (Figure 2).35
 |
Figure 2 The administration of siPHD2-EPCs has been shown to enhance the processes of angiogenesis and neurogenesis following an ischemic stroke. (A) This study presents an illustration of the delivery of Alkyl-SPIO/siPHD2 nanocomplexes into endothelial progenitor cells (EPCs) for the purpose of silencing PHD2. (B) NeuN immunofluorescence staining in the area around the infarct 14 days after EPC transplanting, as well as quantitative data. Scale bar = 20 μm. (C) Representative CD31 immunohistochemical staining in the area around the infarct 7 days after EPC transplanting and quantitative data. Scale bar = 50 μm. *p< 0.05, **p < 0.01, ***p< 0.001. Reprinted from Biomaterials. Volume: 197, Wang C, Lin G, Luan Y, et al. HIF-prolyl hydroxylase 2 silencing using siRNA delivered by MRI-visible nanoparticles improves therapy efficacy of transplanted EPCs for ischemic stroke. 229–243, Copyright 2019, with permission from Elsevier.35 |
Long noncoding RNAs (lncRNAs) have emerged as a crucial element of the genome and have been recognised as significant regulators of angiogenesis.85 Numerous studies have demonstrated a strong correlation between long non-coding RNAs (lncRNAs) and the occurrence of cerebral infarction through the process of angiogenesis.86 Gordon demonstrated that the long non-coding RNA maternally expressed gene 3 (Meg3) has a role in the regulation of cerebral vascular formation. Furthermore, the elimination of Meg3 resulted in an up-regulation of Vegfa and Vegfr2 expression, leading to enhanced angiogenesis.87–89 According to recent research, it has been observed that the downregulation of Meg3 gene expression has a role in facilitating the process of angiogenesis following ischemic events.90 The brain-targeted drug delivery system refers to the method of transporting therapeutically active molecules across the BBB with the intention of treating neurological disorders.91 The application of the anti-TfR antibody, namely OX-26, has the potential to facilitate brain targeting through its binding affinity with TfR. The utilisation of OX26 has been employed in the conjugation of liposome-encapsulated digoxin and nanoparticle-encapsulated loperamide for the purpose of achieving targeted delivery to the brain.36,58,91,92 This approach has demonstrated a favourable therapeutic outcome by means of receptor-mediated endocytosis. The utilisation of PGA as nanodrug carriers has been documented in previous studies, demonstrating its ability to achieve a high rate of DNA packaging while minimising adverse effects.61,62,93,94 In their study, Shen et al developed a non-viral gene therapy vector using PGA as a basic material. This vector was designed to efficiently deliver a plasmid containing Meg3 ShRNA, which is a gene associated with therapeutic effects. Additionally, the vector was attached with OX26 antibody (MPO) to enhance its targeting ability. The researchers evaluated the angiogenesis potential of this vector in vitro and also assessed its efficacy in treating cerebral infarction in vivo. The administration of MPO demonstrated successful localization inside brain tissue, resulting in a notable decrease in the volume of cerebral infarction as observed through TTC staining. Additionally, MPO administration was found to enhance capillary density, as evidenced by HE staining, and promote the growth of micro-vessels within the cerebral cortex, as observed through the immunofluorescence method in vivo. The expression levels of angiogenesis-associated genes Vegfa and Vegfr2 were shown to be increased following the administration of MPO, in comparison to the groups treated with Meg3 or control plasmid.36
One of the endogenous repair mechanisms that takes place following vascular damage caused by a stroke involves the mobilization of human endothelial progenitor cells (hEPCs) produced from the bone marrow. The cells possess the capacity to effectively reach remote destinations and undergo differentiation into fully developed endothelial cells. Specifically, hEPCs are capable of integrating into the developing lining of pre-existing impaired blood arteries (angiogenesis) or stimulating the generation of novel blood vessels (vasculogenesis). Preserving the structural integrity of the cerebral vasculature in a diseased setting is crucial for the viability and potential regeneration of neurons. Blood arteries have a crucial role in facilitating the migration of neuroblasts, which are immature neurons, from their neurogenic niches. Additionally, blood vessels provide a supportive environment for the maturation of these neurons at their original location. Furthermore, blood vessels also contribute to the trophic support of wounded neurons by promoting their proliferation and survival.95 Therefore, the implementation of medicines that improve vascular survival and function has promise for promoting neurogenesis and facilitating brain repair. Nevertheless, the efficacy of these vascular healing systems is not entirely optimal.
Retinoic acid (RA), a metabolic derivative of retinol (vitamin A), exhibits significant bioactivity as a powerful factor. Its signaling mechanism involves the formation of heterodimers between retinoic acid receptor (RAR) and retinoid X receptor (RXR). RAR hetero- and homodimers exhibit an affinity for a specific DNA sequence known as the retinoic acid-response element, thereby facilitating the activation of gene transcription. RA exerts significant regulatory control over the process of neurogenesis by actively facilitating the differentiation of neural stem cells (NSCs).96 Additionally, RA plays a crucial role in angiogenesis by boosting tube formation through the enhancement of VEGF-mediated signaling.97 Nevertheless, when in its unbound state, RA exhibits some constraints, including a diminished ability to dissolve in water and a rapid rate of destruction. Ferreira formulated a polymeric composition consisting of dextran sulphate and polyethylenimine to encapsulate nanoparticles loaded with the chemical RA (RA-NP).37 The application of retinoic acid-loaded nanoparticles (RA-NP) in therapy has demonstrated the potential to effectively and safely facilitate the healing of the ischemic brain by promoting a conducive pro-angiogenic milieu. The RA-NP treatment exhibited an augmentation in endothelial cell proliferation and the creation of tubule networks, while also providing a protective effect against cell death generated by ischaemia. The conditioned media (CM) derived from endothelial cells (EC-CM) that were treated with healthy RA-NP demonstrated a reduction in NSC death and an enhancement in proliferation. Conversely, the CM obtained from ischemic RA-NP-treated endothelial cells exhibited a decrease in cell death, an increase in proliferation, and an induction of neuronal differentiation. Concurrently, hepatocytes were obtained from individuals diagnosed with ischemic stroke. The proliferation of HEPG2 cells treated with RA-NP was shown to be much higher, thereby emphasizing the considerable therapeutic potential of this particular formulation. The RA-NP had a protective effect on endothelial cells against ischemic cell death. Additionally, it induced the release of molecules that promote cell survival and proliferation, as well as cues that facilitate the differentiation of neural stem cells. The study demonstrated that RA-NP exhibited much higher efficiency compared to free RA, with an increase of up to 83-fold. Additionally, the use of RA-NP was found to boost the proliferation of hEPCs. The provided results can be utilized as a foundational basis for the application of RA-NP as vasculotrophic and neurogenic drugs in the context of stroke.37
Numerous recent developments have emerged in the field of angiogenesis following cerebral infarction. These advancements mostly involve the modulation of vascular growth factors, including brain-derived neurotrophic factor (BDNF), and the sonic hedgehog (Shh) signaling protein.98,99 Nevertheless, the administration of pro-angiogenesis factors, such as VEGF, in a singular manner, can potentially result in compromised vascular maturation and heightened permeability of the BBB. This, in turn, can worsen cerebral edema or lead to hemorrhagic transformation.100 The simultaneous administration of extracellular matrix (ECM) integrin ligands and angiogenic agents has been shown to have synergistic effects, suggesting a promising therapeutic approach for enhancing angiogenesis.101,102 Integrins play a crucial role in connecting the ECM to the cytoskeleton. They are engaged in various processes, including the maturation of the vessel lumen, the formation of intercellular tight junctions, and the recruitment of mural cells to the vessels to regulate permeability. Within the integrin family, it has been observed that integrin αvβ3, α5β1, and α3β1 are expressed on endothelial cells. Notably, α5β1 is particularly expressed on the active cerebral vascular endothelium within the ischemic lesion.103,104 The peptide motif Pro-His-Ser-Arg-Asn (PHSRN) has been extensively studied and identified as a binding site for the integrin α5β1. This binding site has been found to have significant downstream effects, including promoting angiogenesis and reducing leakage after myocardial infarction.105,106 Several studies have demonstrated that the pH gradients existing between ischemic and normal tissues are utilized for the purpose of achieving targeted release.107 Nevertheless, the release of medications is constrained by the instability of the surrounding environment and the physiological condition of other bodily components. The shortcomings mentioned can be solved by utilizing nanotechnology-based drug delivery systems that are designed to target many sites simultaneously.108,109 The surface of nanocarriers can be modified by including targeting ligands, which facilitate the precise delivery of medications to the diseased site. Stimulus-responsive nanocarriers facilitate regulated drug release by using the specific attributes of the diseased microenvironment. In their study, Yang et al present a straightforward approach to fabricate integrin ligand-conjugated, pH-responsive dual-targeted nanoparticles, which can be utilized for efficient drug administration to the ischemic brain (Figure 3).8 Hydroxyethyl starch (HES), a water-soluble polysaccharide commonly used as a volume expander in clinical settings, was employed as a nanocarrier platform.110,111 The utilization of the upregulated expression of integrin α5β1 on the endothelial cells of cerebral blood vessels in ischemic brain tissue allows for the targeted delivery of therapeutic agents to areas affected by cerebral ischemia through the use of PHSRN-HES, a ligand-mediated approach. We additionally employed pH-dependent electrostatic adsorption to PHSRN-HES for the purpose of delivering smoothened agonist (SAG), a potent activator of the Shh signaling pathway, which in turn facilitates the processes of angiogenesis and neuroplasticity. The acidic ischemia zone experiences a notable decline in ambient pH, which therefore diminishes the electrostatic adsorption capacity. This reduction in capacity may facilitate the release of SAG in the aforementioned acidic ischemic region. In addition, the researchers provided evidence that the administration of SAG@PSHRN-HES had a substantial impact on the promotion of angiogenesis and the reduction of vascular permeability. Moreover, this intervention was found to enhance neuroplasticity and facilitate neurological recovery following ischemic stroke.8
 |
Figure 3 The structure of SAG@PHSRN-HES and its use for active cerebral vasculature-targeting and pH-sensitive therapy of ischemic stroke are depicted schematically. Reproduced with permission from Yang H, Luo Y, Hu H, et al. pH-Sensitive, cerebral vasculature-targeting hydroxyethyl starch functionalized nanoparticles for improved angiogenesis and neurological function recovery in ischemic stroke. Adv Healthc Mater. 2021;10(12):e2100028. © 2021 Wiley-VCH GmbH.8 |
The process of angiogenesis, which involves the generation of new vessels from pre-existing vasculature, is responsible for driving revascularization.112 The process of angiogenesis is launched promptly following an ischemia injury by the production of angiogenic factors, including as platelet-derived growth factor receptor beta, VEGF, and insulin-like growth factor binding proteins, by cells in response to exposure to a hypoxic environment.112–115 The process of angiogenesis is shown to be fully active within a span of three days following an injury, as evidenced by the initiation of vasculature development in the peri-infarct region. The longevity of these newly created vessels, similar to newborn neurons generated in response to a stroke, is limited within the post-stroke milieu.116,117 According to existing literature, it has been proposed that this particular mechanism may primarily serve to facilitate the removal of cellular debris rather than being primarily aimed at long-term regeneration endeavors.116–119 Nevertheless, it is worth noting that angiogenesis frequently occurs in conjunction with neurogenesis, as the areas where new blood vessels form often coincide with regions containing actively dividing neural progenitor cells.116,117 Consequently, the sustained promotion of angiogenesis may potentially enhance neurogenesis, thereby potentially augmenting reparative mechanisms and enhancing functional recuperation following a stroke.116,117,120 In order to enhance angiogenesis and optimize brain targeted delivery, researchers have developed neurogenesis-based nanoparticles that aim to provide superior results in the context of ischemic stroke.
In a clinical context, the restoration of blood flow, known as reperfusion, is accomplished through the administration of recombinant human tissue-type plasminogen activator (tPA), which is the sole treatment approved by the United States Food and FDA for ischemic stroke. Nevertheless, the administration of tPA beyond approximately 4.5 hours after the occurrence of a stroke is considered unsafe.121 This is mostly owing to the heightened likelihood of hemorrhagic complications, the disruption of the blood-brain barrier, as well as the neurotoxic impacts of tPA.122,123 While reperfusion following tPA therapy facilitates the delivery of oxygen and nutrients to the ischemic tissue, it also triggers an augmented generation of ROS by ischemic neuronal and glial cells, invading neutrophils, and vascular cells that make up the BBB.124–126 Recent investigations have shown in vivo evidence of neurogenesis in the adult mammalian brain.127 Previous studies have demonstrated that endogenous neural precursor cells (NPCs) undergo activation subsequent to a stroke event. These NPCs subsequently undergo maturation and migration towards the location of the lesion, where they subsequently develop into neuronal cells.128 Indeed, Huang et al have demonstrated a significant decrease in neurogenesis in mice defective in superoxide dismutase (SOD) and suffering from brain injury generated by radiation.129 Petro designed a strategy wherein the antioxidant enzymes catalase (CAT) and SOD are encapsulated in nanoparticles (referred to as nano-CAT/SOD) and administered immediately after tPA delivery during reperfusion. The aim of this approach is to counteract the excessive formation of ROS and thereby prevent the subsequent cascade of inflammatory and degenerative processes. By creating a favorable environment, this intervention may facilitate the activation and mobilization of progenitor cells, ultimately promoting the endogenous mechanisms of neurogenesis in the infarcted region.38 The researchers discovered that the negative impact of tPA and the excessive production of ROS resulting from a stroke can be mitigated through the administration of tPA+ nano-CAT/SOD. This is supported by the observed augmentation in the presence of nestin- and SOX2-positive cells. The findings of these investigations demonstrate that the administration of tPA+ nano-CAT/SOD not only alleviates the suppressive impact of tPA on neurogenesis but also counteracts the detrimental influence of ROS generated during stroke event (Figure 4).38
 |
Figure 4 Increasing the amounts of biological markers (Nestin, GFAP and SOX2) and restoring the movement and activity of NPCs show that giving SOD-CAT-PLGA-NPs with tPA improved neurogenesis after stroke. (A-D) Immunofluorescence was used to identify the expression of GFAP (A), SOX2 (B), and DAPI (C) in different groups of the subventricular zone and rostral migratory stream. The resulting figures were merged (D). (E) Immunohistochemical analysis was used to identify the expression of Nestin in different groups of the subventricular zone and the rostral migratory stream. Scale bar = 50 mm. Reprinted from Biomaterials. Volume: 81, Petro M, Jaffer H, Yang J, Kabu S, Morris VB, Labhasetwar V. Tissue plasminogen activator followed by antioxidant-loaded nanoparticle delivery promotes activation/mobilization of progenitor cells in infarcted rat brain. 169–180, Copyright 2022, with permission from Elsevier.38 |
The ROS that has built up in the brain area also causes harm to intracellular macromolecules such as lipids, proteins, and nuclear acids. This damage leads to the initiation of apoptosis and the inhibition of neurogenesis following stroke.130,131 According to a paper, resveratrol (RES), a natural polyphenol with potential benefits, has been found to mitigate damage and apoptosis generated by ROS, hence promoting neurogenesis.132 Nevertheless, the utilization of this substance was limited due to its short half-life, lack of solubility in water, and low concentration in the brain.133 Lu et al demonstrated that the use of polymeric nanoparticles, specifically those encapsulating resveratrol (RES-NPs), as carriers for drug delivery exhibited significant neuroprotective effects on cultured neurons. The encapsulation of resveratrol within the nanoparticles, which were composed of Poly (N-vinylpyrrolidone) -b-poly(ε-caprolactone), resulted in improved uptake of the drug, enhanced clearance of ROS, and a superior anti-apoptotic effect compared to the administration of free resveratrol.134 Subsequent research conducted by the authors revealed that the use of RES-NPs through the intra-carotid artery route yielded significant mitigation of cerebral ischemia-reperfusion damage in rats subjected to middle cerebral artery occlusion (MCAO).39 The disruption of the BBB caused by ischemia-reperfusion resulted in the leaking of albumins, as evidenced by the presence of evans-blue dye, and the development of cerebral edema. The administration of RES-NPs had a strong protective effect on the integrity of the BBB by reducing the extent of ischemia-reperfusion damage. In addition, it was shown that RES-NPs exhibited a reduction in oxidative stress after reperfusion, as well as a suppression of neuronal death and an enhancement of neurogenesis.39
Inorganic Nanoparticles
The majority of neuroprotective medications are ineffective in salvaging neurons from cerebral ischemia shocks mostly due to their focus on mitigating downstream cascading processes, including excitotoxicity, reactive oxygen species (ROS) and nitrosative stress, and inflammation, rather than addressing the underlying hypoxia that occurs first.26 Research has demonstrated that metallic nanoparticles has the ability to act as scavengers of ROS and hypoxia, hence promoting the process of angiogenesis.
According to the paper, inorganic nanoparticles have been found to provide protection against ischemic stroke in a live animal model, such as cerium oxide nanoparticles (CeO2 NPs) and zinc oxide nanoflowers.135–137 The potential great antioxidant ability of CeO2 NPs has garnered significant attention in scientific research, mostly attributed to the creation of oxygen vacancies and low valence states.138 Dl-3-n-butylphthalide (NBP) is a novel chemical compound that belongs to class I drugs. It was developed in China and has received approval from theFDA for Phase II clinical trials in the management of ischemic stroke.139 NBP was initially derived from the seeds of celery, demonstrating potential in enhancing microcirculation inside the ischemic brain region. It has been found to facilitate angiogenesis, neurogenesis, and neuroplasticity, while also inhibiting inflammation, reducing apoptosis, and exhibiting a clear neuroprotective impact on ischemic stroke.140–142 In their study, Li et al employed CeO2 nanoparticles (NPs) as carriers for drug delivery and utilized NBP to explore a novel therapeutic avenue for the management of ischemic stroke (Figure 5).40 Ultrasmall cerium dioxide nanoparticles (CeO2 NPs) with an approximate diameter of 5 nm were manufactured using a high-temperature technique. These nanoparticles were subsequently coated with polyethylene glycol (PEG) to facilitate the loading of NBP drugs. The cerium oxide nanoparticles loaded with NBP, referred to as NBP-CeO2 NPs, exhibit a remarkable capacity for scavenging ROS in vitro during oxygen-glucose deprivation/reoxygenation (OGD/R). Furthermore, these nanoparticles effectively restore the impaired mitochondria. Additionally, the mitigation of BBB damage and neuronal apoptosis was seen through the preservation of mitochondrial shape and function. In the mouse model of MCAO, the administration of NBP-CeO2 nanoparticles demonstrated the ability to restore impaired mitochondria and mitigate the disruption of the BBB. Consequently, this intervention significantly ameliorated cerebral infarction and cerebral edema, while also inhibiting neuroinflammation and neuronal death. The results of long-term research indicate that the co-administration of NBP (N-butylphthalide) with CeO2-NPs effectively stimulates angiogenesis and substantially ameliorates impairments in nerve function following ischemic stroke.40
 |
Figure 5 Ultra-small cerium oxide nanoparticles loaded with NBP (NBP-CeO2 NPs) attenuated BBB disruption and promoted angiogenesis. (A) The utilization of NBP-CeO2 NPs, which are extremely small nanoparticles of cerium oxide loaded with NBP, effectively combines antioxidant and neurovascular beneficial effects to mitigate brain damage caused by ischemic stroke. (B) CD31 immunofluorescence labeling on brain slices 14 days after MCAO/R detected cerebral microangiogenesis in each group. (C) CD31 relative fluorescence intensity was statistically evaluated. ***p < 0.001 vs MCAO/R group; ##p < 0.01. Scale bar = 50 μm. Reprinted from Biomaterials. Volume: 291, Li X, Han Z, Wang T, et al. Cerium oxide nanoparticles with antioxidative neurorestoration for ischemic stroke. 121904, copyright 2022, with permission from Elsevier.40 |
Given that hypoxia is a major concern following a stroke, it is crucial to explore therapeutic interventions that can consistently deliver oxygen to help ameliorate the adverse microenvironment. Such interventions have the potential to successfully safeguard neurons against the detrimental effects of cerebral ischemia insults.143 Synechococcus elongatus (S. elongatus), a unicellular cyanobacterium that is an obligate photoautotroph, has been employed in recent research to enhance tissue oxygenation and enhance heart function as a potential treatment for ischemia myocardium.144–146 In addition, a distinct variety of cyanobacterium has been demonstrated to enhance oxygen concentrations within hypoxic regions of tumors.147 S. elongatus exhibits the capacity to continuously generate oxygen and consume carbon dioxide under illumination, which suggests its potential to address the constraints associated with oxygen-carrying biomaterials. Consequently, it could serve as an effective component for oxygen generation and carbon dioxide consumption. Additionally, an additional practical obstacle encountered in stroke photosynthetic therapy pertains to the efficient delivery of light for facilitating photosynthesis in S. elongatus within cerebral ischemia zones located beneath the cranium. Despite the impressive tissue penetration capabilities of near-infrared light (NIR) with a wavelength of 808 nm,148,149 it is not directly applicable for photosynthesis.150,151 The potential use of upconversion nanoparticles (UCNPs) in converting NIR into visible light, which is essential for the photosynthesis of S. elongatus, suggests that the combined application of S. elongatus and UCNPs could be a viable strategy for implementing the suggested photosynthesis-based treatment for stroke.152,153 In their study, Wang et al documented the creation of a nanophotosynthesis treatment (NPT) through the utilization of a core-shell structure consisting of Nd3+-doped UCNPs. This structure was designed to transform near-infrared (NIR) light with a wavelength of 808 nm into visible light, which in turn stimulated S. elongatus to generate oxygen. The resulting oxygen production had a protective effect on neurons, shielding them from ischemia insults.41 The full characterization of S. elongatus encompassed its biocompatibility, capacity for oxygen generation, and neuroprotective effects. Despite the presence of a barrier formed by the skull, the NIR that was transformed by UCNPs proved to be adequate in activating S. elongatus. This activation resulted in the production of oxygen and the simultaneous reduction of carbon dioxide levels. Consequently, the survival of neuronal cells that had experienced injury generated by OGD was enhanced. In an animal model of stroke known as MCAO, the administration of this NPT resulted in improved oxygenation of the affected brain tissues, increased survival of neurons, decreased volumes of the infarcted areas, and enhanced the formation of new blood vessels (angiogenesis). These combined effects led to a substantial restoration of neuronal functions and improved behavioral performance in the animals (Figure 6).41
 |
Figure 6 NPT decreased inflammation and promoted angiogenesis poststroke. (A) Schematic Depiction of the Therapeutic Approach Utilising Nano-Photosynthesis. (B) Representative fluorescence images of vessels in the infarct and peri-infarct 8 weeks after the mice received different treatments. The infarct zones were outlined by white dashed lines. (C-D) Quantification of percentages of CD31 positive area in the infarct and peri-infarct, respectively. **p<0.01. Scale bar = 50 μm. Reproduced with permission from Wang J, Su Q, Lv Q, et al. Oxygen-generating cyanobacteria powered by upconversion-nanoparticles-converted near-infrared light for ischemic stroke treatment. Nano Lett. 2021;21(11):4654–4665. Copyright 2022, American Chemical Society.41 |
Liposomes
Liposomes have emerged as a promising drug delivery technology in the field of clinical translation due to its notable advantages, including strong biocompatibility, minimal toxicity, and substantial capacity for encapsulating diverse cargos.154 Furthermore, liposomes has certain advantages in the context of medication delivery following a stroke, as they have the ability to selectively cluster in the ischemic hemisphere, resulting in a greater accumulation of therapeutic agents.155 Moreover, it has been discovered that 48 hours following a stroke, there is a biphasic barrier enhancement and the presence of tight junction anomalies. These factors contribute to an increase in the paracellular permeability of molecules and liposomes. Furthermore, the involvement of caveolin-mediated endocytosis and the heightened rate of transcytosis significantly enhance the transcellular transportation of liposomes within a mere 6 hours following reperfusion, and this effect continues for a minimum of 24 h.25,156
Ginkgolide B (GB) exhibits potent efficacy in the treatment of cerebrovascular diseases. It achieves this by inhibiting inflammatory responses through its involvement in platelet-activating factor mediated signal transduction. Additionally, GB mitigates neuronal damage by modulating the miR-206/BDNF signaling pathway.157,158 Additionally, it has been observed that GB exerts a beneficial influence on the process of neural stem cell differentiation following a stroke. This effect is achieved by the overexpression of SOCS2, which subsequently enhances the activation of the EGF receptor.159 Nevertheless, the LogP value of GB is merely 0.146, indicating a limited degree of hydrophilicity and lipophilicity. Consequently, the formulation of GB in liposomes is challenging due to its inadequate encapsulation efficiency and stability, as stated in reference.42 In order to address the issue of GB’s low lipophilicity, Li put forth solutions aimed at the formation of covalent complexes with polyunsaturated fatty acids (PUFA) and subsequent encapsulation within liposomes. The selection of docosahexaenoic acid (DHA) was based on its capacity to be incorporated into the lipid bilayer, resulting in enhanced stability of the complex.160 The researchers Li et al initially synthesized GB-DHA in order to enhance the lipophilicity of GB. Subsequently, they encapsulated GB-DHA into liposomes to augment its potential to target the brain.42 The liposomes possess the ability to specifically target the ischemic hemisphere of the brain, resulting in a collaborative protective effect against neuron apoptosis. This is achieved through the elimination of ROS, the remodeling of the neurovascular unit by regulating the polarization of microglia towards an anti-inflammatory phenotype, and the facilitation of anti-inflammatory activity by reducing the infiltration of peripheral immune cells. The involvement of the apoptotic pathway in the neuroprotective mechanism of Lipo@GB-DHA was observed in rats subjected to MCAO. An increased amount of BDNF, known to promote the development of neurons through the Wnt/β-catenin pathway, was seen in the brains of rats treated with Lipo@GB-DHA.161 The findings indicated that Lipo@GB-DHA has the potential to promote both neuronal development and angiogenesis.42
Biomimetic Nanoparticles
The utilization of targeted nanomedicines has demonstrated extensive potential in the management of stroke. Nevertheless, one drawback is the exogenous nature of the feature, which poses a potential risk of clearance by the reticuloendothelial system. In order to address this limitation, many approaches using bionic nanomedicine delivery systems incorporating cells, cell membrane vesicles, and exosomes have been extensively suggested. The utilization of naturally occurring nanoparticles within biological systems has been employed to create novel structures that enhance the development of delivery systems through the utilization of inherent targeting capabilities.162 Biomimetic systems have demonstrated considerable utility in the field of biomedicine, namely in applications like as drug delivery, gene transport, theranostics, and biosensing. This is mostly due to their exceptional biocompatibility, little toxicity, and notable interactive properties.
Extracellular vesicles (EVs) are small vesicles that encompass proteins, lipids, and genetic elements, and they exert a significant influence on intercellular communication.163 Presently, the administration of EVs-based therapy primarily involves the intravenous injection of EVs into animals affected by stroke. However, this approach is not ideal for various reasons. One such reason is that intravenously injected EVs tend to accumulate primarily in the liver, lung, and spleen, with limited delivery to the brain. Additionally, the lack of effective protection in the in vivo circulation leads to the degradation and subsequent loss of EVs.164 Given the necessity for prolonged angiogenesis and neurogenesis in the recovery of brain function, there is an immediate requirement for the development of a new biocompatible scaffold. This scaffold should enhance the retention of EVs in the damaged brain area and facilitate the sustained release of EVs within the brain lesion following a stroke. By doing so, the scaffold would extend the bioactivity of EVs and expedite the process of neural regeneration.164
Stem cells are a class of cells characterized by their high degree of undifferentiation, as well as their capacity for self-renewal and ability to develop into several cell types. Various sources of stem cells have been suggested for the therapy of ischemic stroke, such as NSCs, mesenchymal stem cells (MSCs), induced pluripotent stem cells (iPSCs), and EPCs. Among these, NSCs and MSCs have received the most extensive attention in the literature.165 Nevertheless, the adverse microenvironment associated with ischemic stroke has been found to significantly diminish the viability and proliferative capacity of stem cells, hence imposing substantial constraints on their therapeutic efficacy.166 MSCs, whether in their original form or with alterations, have demonstrated significant promise in enhancing the formation of new blood vessels (angiogenesis) in both preclinical studies of ischemic diseases and clinical trials.167–169 However, the utilization of MSCs derived from various tissues such as bone marrow, adipose tissue, umbilical cord, muscle, dental pulp, etc., for cell-based therapy is accompanied by certain limitations. These limitations include the invasive nature of the procurement procedure, restricted potential for cell proliferation, functional decline associated with aging, and the potential risk of rejection when transferring cells from a different individual.170,171 Consequently, these limitations hinder the broader clinical applications of MSCs. The successful generation of induced pluripotent stem cells (iPSC) from adult somatic cells of patients has been made possible with the development of reprogramming techniques. The stability of small extracellular vesicles (sEV) surpasses that of stem cells across diverse physiological settings, rendering them highly suited for therapeutic interventions in the context of ischemic stroke. Moreover, sEV possess the advantageous ability to readily traverse the BBB, further enhancing their potential as a therapeutic modality.172,173 A recent study has provided evidence that tiny extracellular vesicles, specifically those released by mesenchymal stem cells generated from human induced pluripotent stem cells (iMSC-sEV), had the ability to mitigate limb ischemia through the facilitation of angiogenesis.174 There exists a positive correlation between angiogenesis and the recovery of cerebral function following a stroke.175 In their study, Xia et al (year) observed that the infarct boundary zone exhibited the presence of freshly created vasculature and mature vessels, as evidenced by the positive staining of CD31/EdU, CD34, and CD31.43,176 The experimental group of vehicles shown a statistically significant increase in the presence of CD31+/EdU+ and CD34+ endothelial cells compared to the control group, indicating the activation of a natural protective response including spontaneous angiogenesis following a stroke. It is worth mentioning that there was a significant increase in the number of CD31+/EdU+ and CD34+ cells observed in the iMSC-sEV group compared to the vehicle group. This finding suggests that the administration of iMSC-sEV after a stroke has a positive effect on promoting angiogenesis (Figure 7).43
 |
Figure 7 iMSC-sEV promote angiogenesis following stroke and increase HUVEC migration and tube formation after OGD. (A–D) Seven days after MCAO, angiogenesis was evaluated by immunofluorescence staining of CD31/EdU and CD34. Scale bar = 100 μm. *P < 0.05. Reproduced from Xia Y, Ling X, Hu G, et al. Small extracellular vesicles secreted by human iPSC-derived MSC enhance angiogenesis through inhibiting STAT3-dependent autophagy in ischemic stroke. Stem Cell Res Ther. 2020;11(1):313. Creative Commons.43 |
Mesenchymal stromal cell-derived extracellular vesicles (MSC-sEVs) obtained from the supernatants have demonstrated the ability to enhance neurological recovery and facilitate brain remodeling following focal cerebral ischemia in both rats and mice, as evidenced by studies.177–180 The impact of MSC-sEVs on microvessels is heavily influenced by the specific tissues and pathophysiological conditions present. The impact of MSC-sEV preparations on angiogenesis in cancer tissues varies depending on the specific source of MSCs and the tumor microenvironment.126,181,182 However, it has been observed that MSC-sEVs can enhance the proliferation and tube formation of cultured human umbilical vein endothelial cells (HUVECs) in a manner that is dependent on HIF-1α.183 Gregorius conducted an assessment of the impact of MSC-sEVs on the in vitro proliferation, migration, and tube formation of human cerebral microvascular endothelial cells. Additionally, the study examined the effects of MSC-sEVs on post-ischemic angiogenesis, brain remodeling, and neurological recovery following MCAO in mice.44 In additional investigations, mice subjected to intraluminal MCAO were also administered EV preparations derived from either normoxic mesenchymal stem cells, hypoxic MSCs, or cell culture media. Within certain subgroups, the polymorphonuclear neutrophil leukocytes (PMN), which have previously demonstrated their role in facilitating the acute neuroprotective effects of MSC-sEVs,180 were observed to be depleted. The study conducted by Gregorius et al demonstrated that sEVs derived from mesenchymal stem cells subjected to hypoxic conditions, as opposed to MSCs at normal oxygen levels or the culture media alone, exhibited the ability to stimulate angiogenesis. The administration of hypoxic MSCs resulted in an augmentation of microvascular length and branching point density inside previously ischemic tissue, as determined through the utilization of 3D light sheet microscopy over a period of up to 56 days. The in vivo induction of angiogenesis by sEVs was found to be contingent upon the presence of PMN. Using anti-Ly6G antibodies, they simultaneously reduced PMN numbers in two subsets. The administration of MSC-sEVs did not have an impact on microvascular remodeling in mice that had been deprived of neutrophils. The sEVs generated from MSCs under hypoxic conditions exhibit unique characteristics related to angiogenesis, as depicted in Figure 8. The regenerative benefits of MSC-sEVs are enhanced by hypoxic preconditioning.44
 |
Figure 8 When PMNs are absent in vivo, sEVs produced from hypoxic MSCs promote microvascular remodeling after ischemic stroke. (A–C) The microvascular network properties in the ischemic cerebral cortex were examined using 3D light sheet microscopy in mice that were subjected to 40 minutes of MCAO and then survived for 14 days. A, microvascular length density; B, branch point density; and C, mean branch length. (D) Magnified axial views of the striatum and cortex in an ischemic mouse brain showing the regions of interest for determining the properties of the microvascular network. Images of the ischemic cortex taken using maximum intensity projection (E) from each of the five groups. *p <0.05 compared with isotype/vehicle; #p <0.05 compared with isotype/sEVhypoxic. Scale bars=500 µm (in (D)/100 µm (in (E). Reproduced from Gregorius J, Wang C, Stambouli O, et al. Small extracellular vesicles obtained from hypoxic mesenchymal stromal cells have unique characteristics that promote cerebral angiogenesis, brain remodeling and neurological recovery after focal cerebral ischemia in mice. Basic Res Cardiol. 2021;116(1):40. Creative Commons.44 |
Recent experimental studies have suggested that acid sphingomyelinase (ASM), known as Asm for the murine protein and shortened ASM for the human enzyme, plays a crucial role in facilitating the effects of antidepressant drugs.184 ASM catalyzes the hydrolytic cleavage of sphingomyelin, resulting in the formation of ceramide. Ceramide is an essential component of membrane microdomains, which play a crucial role in regulating many cell signaling processes.185 In a theoretical framework of stress-induced depression characterized by unpredictability, the administration of antidepressant medications such as amitriptyline and fluoxetine shown inhibitory effects on cerebral Asm activity. Furthermore, these medications were found to repair the processes of neuronal proliferation and differentiation in the hippocampus, ultimately leading to a reversal of depressive-like behaviors.186 In the absence of ASM, the administration of antidepressants failed to induce an increase in neuronal proliferation and differentiation, and did not effectively alleviate depressed symptoms.186 After experiencing localized and global cerebral ischemia, studies have demonstrated an elevation in Asm activity and ceramide levels within the brains of ischemic mice and rats.187–190 Following MCAO, the presence of hereditary Asm deficiency was observed to result in a decrease in infarct volume, neurological impairments, and the abundance of proinflammatory cytokines during the acute phase of stroke, namely within 24 hours after the occurrence of the stroke.190 Yusuf demonstrated a notable rise in Brain ASM activity following ischemia/reperfusion, which aligns with the observed elevation of ceramide levels in microvessels.45 The administration of amitriptyline resulted in the suppression of ASM activity, leading to a decrease in ceramide levels. Additionally, it was observed that there was an increase in microvascular length and branching point density in wildtype mice, but not in ASM-deficient mice (Smpd1−/−). These effects were evaluated using 3D light sheet microscopy. In the context of cellular cultivation, the administration of amitriptyline, fluoxetine, and desipramine resulted in an augmentation of endothelial tube formation, migration, as well as an increase in the abundance of VEGFR2 and the release of VEGF. The observed effect was nullified through the process of Smpd1 knockdown. The researchers discovered that the facilitation of angiogenesis using ASM inhibitors was facilitated by the production of sEVs from endothelial cells. These sEVs demonstrated an increased absorption in target cells. In an in vivo setting, the augmented process of angiogenesis resulting from the release of sEVs by ASM inhibitors was shown to be accompanied by a reaction in brain remodeling. This response was characterized by an enhancement in the integrity of the blood-brain barrier, a decrease in the infiltration of leukocytes, and an increase in the survival of neurons.45
The potential therapeutic implications of microglia are of great interest, particularly in light of prior research that has shown improved neurological recovery in animals treated with microglia preconditioned with OGD at an early stage of stroke.191 The microglia exhibit a discernible alteration in their protein profiles, characterized by elevated amounts of the transforming growth factor-β (TGF-β).191 Elevated concentrations of TGF-β during the initial stages of a stroke event have the potential to trigger signaling cascades that promote anti-inflammatory responses and a shift towards M2 polarization inside the ischemic brain.191–194 The effectiveness of cell-based therapies, such as microglia transplantation, is currently hindered by two main challenges: limited biodistribution of the transplanted cells and the risk of cell embolism or tumor formation.195–197 Prior research has indicated that the therapeutic efficacy of EVs derived from various stem cell origins is comparable to that of the parent cells. These EVs have been found to possess similar beneficial properties as their respective host cells, as supported by previous studies.164,198–201 The work conducted by Zhang et al examines the therapeutic effects of EVs obtained from microglia that were preconditioned with OGD in both in vitro and in vivo models of stroke. The researchers also discovered that the transportation of EVs from microglia that were preconditioned with OGD could potentially promote the formation of new blood vessels (angiogenesis) and prevent programmed cell death (apoptosis) in the brain affected by ischemia.46 A comprehensive examination of the relationship between the cell proliferation marker BrdU and the endothelial cell marker CD31 demonstrated a notable rise in the levels of BrdU+/CD31+ cells within the ischemic striatum on the seventh day following ischemia in animals subjected to EVs treatment. However, this observation was not corroborated in mice treated with TGF-β1 siRNA-transfected microglia (si-EVs). Similarly, the injection of EVs had a notable impact on reducing rates of ischemia cell death. However, it was observed that the treatment of si-EVs derived from TGF-β1 knockdown microglia did not have any effect on the number of TUNEL+ apoptotic cells per mm2.46
In recent studies, researchers have investigated the mechanical extraction of the cell-free liquid fraction, known as fat extract (FE), from human adipose tissue.202,203 The cell-free fraction, known as FE, offers advantages in terms of safety by circumventing problems associated with cellular components, and also demonstrates enhanced clinical applicability. In comparison to stem cells, FE exhibit advantages in terms of collection ease, extended storage capacity, and reduced immunogenicity.203 Moreover, FE encompasses a diverse range of angiogenic factors such as VEGF, TGF-β, basic fibroblast growth factor, and glial cell line-derived neurotrophic factor, among others. The administration of FE has been shown to augment the viability of fat grafts in mice by exerting proangiogenic, anti-apoptotic, and pro-proliferative effects. Additionally, FE has demonstrated the ability to enhance angiogenesis in a hindlimb ischemic model.202 Neutrophil membrane-derived nanovesicles that are loaded with Resolvin D2 have the ability to specifically target sites of inflammation and improve retention, hence providing protection against brain damage in the context of ischemic stroke.204 Among the various particles coated with membranes, platelets coated nanoparticles have demonstrated distinctive targeting capabilities. Initially, it is worth noting that platelet-like particles (PLTs) possess a circulation half-life of roughly 30 hours. This extended duration can be attributed to the presence of CD47, a protein that effectively inhibits immune clearance mechanisms. Furthermore, it should be noted that platelets (PLTs) exhibit a diverse range of receptors, including integrins and selectins, which play a crucial role in their ability to dynamically adhere to injured blood vessels.205 The membrane-coated nanoparticles of PLTs possess extensive and dynamic biointerfacing properties, rendering them highly appealing as drug carriers for the purpose of targeted administration to inflamed blood arteries.206,207 Wang developed a nanoparticle system composed of PLTs membrane-coated PLGA nanoparticles, encapsulating FE and coupled with RGD peptide, referred to as RGD-PLT@PLGA-FE. This system was designed to facilitate the specific delivery of FE to the infarct region in mice affected by stroke.47 In this study, RGD-PLT@PLGA nanoparticles were employed as a vehicle for the targeted delivery of FE, with the aim of facilitating angiogenesis and neurogenesis for the purpose of brain repair in cases of injury. The nanoparticles exhibited an extended circulation period and actively targeted the ischemic stroke regions due to the mimicking features of the PLTs membrane and RGD peptides. Furthermore, the biodegradability of PLGA allows for the sustained release of FE, which can be utilized in the treatment of stroke. The administration of targeted and sustained release nanoparticles to the ischemic region resulted in the augmentation of angiogenesis and neurogenesis, leading to a notable improvement in the therapeutic effectiveness for ischemic brain conditions. The data presented in this study indicate that the administration of RGD-PLT@PLGA-FE resulted in a significant enhancement of angiogenesis and neurogenesis in mice with stroke (Figure 9).47
 |
Figure 9 RGD‑PLT@PLGA targets brain and promotes angiogenesis and neurogenesis of stroke mice. (A and B) Pictures showed CD31+ microvessels in the peri‑infarct region at 14 days after stroke. (C) Pictures showed CD31+ /Ki67+ cells in the peri‑infarct region at 14 days after stroke. (D) Pictures showed DCX+ cells in the subventricular zone at 14 days after stroke. (E) Quantitative analysis of the number of blood vessels of mice that treated with 10% sucrose and other tested groups at 14 days after stroke at 14 days after stroke. (F) Quantitative analysis of the number of CD31+/Ki67+ cells of mice that treated with 10% sucrose and other tested groups at 14 days after stroke. (G) Quantitative analysis of DCX+ cells in the subventricular zone of mice that treated with 10% sucrose and other tested groups at 14 days after stroke.at 14 days after stroke. *p< 0.05, **p < 0.01, ***p< 0.001. Adapted from Wang C, Yang X, Jiang Y, et al. Targeted delivery of fat extract by platelet membrane-cloaked nanocarriers for the treatment of ischemic stroke. J Nanobiotechnology. 2022;20(1):249. Creative Commons.47 |
Limitation of Nanoparticles
Polymeric nanoparticles show potential for targeted medication delivery, however they have drawbacks such as high cost and intricate production processes. In the laboratory, it is possible to prepare nanoparticles that have a high drug loading capacity and good stability. However, when it comes to large-scale production, there are limitations imposed by environmental factors and other constraints. As a result, it may not be feasible to produce nanoparticles of the same quality and specifications, which means they may not fully meet the requirements for clinical drug delivery. Therefore, it is necessary to conduct a comprehensive investigation into the many characteristics of polymer nanoparticles in order to regulate the chemical and physical properties of these nanoparticles for effective treatment of ischemic stroke.
Furthermore, there exist inorganic nanoparticles that have considerable potential in post-stroke treatment owing to their intrinsic characteristics. Preclinical investigations have consistently demonstrated that nanoparticles tend to aggregate in the kidney, liver, spleen, and brain following their injection, hence posing potential risks of systemic toxicity. It is important to continue studying the way in which inorganic nanoparticles, such as iron nanoparticles, gold nanoparticles, and other metal nanoparticles, are processed by the human body’s metabolism. Prolonged accumulation of these substances in the brain can initiate neuronal death, mitochondrial malfunction, neuroinflammation, and other forms of harm. Even nanoparticles that are capable of degradation can cause neurotoxicity. When test animals were injected with chitosan nanoparticles modified with polysorbate 80, the body weight of the experimental animals consistently fell over a period of 7 days. This decrease in body weight was shown to be dependent on the dosage and had an influence on cell activity.7 Neuronal loss in chicken embryos is induced by magnetic iron oxide nanoparticles, but cerium oxide nanoparticles hinder the development of neural stem cells.208 Inorganic non-metallic nanoparticles such as carbon nanotubes, graphene, and silica nanoparticles have been utilised for stroke treatment.209 It is important to acknowledge that the majority of inorganic non-metallic compounds, excluding silica, have the capacity to be biotoxic, but silica has shown both biocompatibility and degradability. The brain has difficulty metabolising most inorganic non-metallic materials, leading to their accumulation. This accumulation can cause redox alterations, apoptosis, autophagy, reduced lysosomal activity, cytoskeletal impairment, and disturbance in vesicle trafficking. Additionally, maintaining the stability of these inorganic nanomaterials in solution is a significant challenge.
In general, liposomes have excellent drug loading capacity, drug protection capabilities, and great biocompatibility. Nevertheless, its application in stroke therapy is hindered by the drawback of limited precision in targeting. Research has shown that the capacity of liposomes to target the brain may be enhanced by attaching PEG, altering the surface charge, or attaching particular targeting ligands. This, in turn, improves the effectiveness of the treatment. Nevertheless, as a developing technology, concerns regarding the compatibility of biomimetic nanoparticles with living organisms persist and require ongoing investigation and enhancement. Furthermore, the majority of biomimetic nanoparticles utilised in the diagnosis and treatment of brain illnesses are still in the preclinical stage. However, there is a paucity of further clinical data that would aid in the process of translating them into clinical practice. Furthermore, it is imperative to take into account the material toxicity of the nano delivery system itself.15 We must prioritise our emphasis on ensuring the stability of nano-drug delivery systems. These systems need stringent manufacturing and storage conditions to sustain stability, and ensuring their long-term stability over lengthy durations necessitates comprehensive studies.
Conclusions and Perspectives
The absence of a viable therapeutic approach for angiogenesis in stroke has been a significant barrier for healthcare professionals and individuals affected by ischemic stroke, both in terms of therapy and long-term recuperation. The BBB poses a significant challenge in delivering therapeutic medicines to cerebral ischemia areas due to its unique properties. The lack of targeted delivery of therapeutic medications to ischemia areas leads to unfavorable clinical outcomes. In recent times, there has been a significant utilization of nanoparticles in the management of stroke. This adoption has been driven by the observed enhancement in the efficacy of conventional pharmaceuticals and the potential it offers for the implementation of developing therapeutic approaches, including gene therapy, targeted therapy, and treatment visualization.210 The angiogenic processes and progression of ischemic stroke are influenced by a variety of nanoparticles. These nanoparticles encompass the encapsulation of pro-angiogenic proteins within appropriate polymeric nanoparticles, the development of nanocarriers that can selectively penetrate the blood-brain barrier, the utilization of polymeric nanoparticles, the use of stimulus-responsive nanocarriers, the application of upconversion nanoparticles, the internalization of nanoparticles through transcellular transport via endocytosis, and the utilization of biomimetic nanoparticles, among others. The researchers have developed many therapeutic strategies utilizing functional nanoparticles to promote angiogenesis in ischemic zones. The nanoparticles primarily consist of brain-targeting nanoparticles, BBB therapy nanoparticles, BBB penetration-enhancing nanoparticles, BBB-protective nanoparticles, and nanoparticles that utilize endocytosis for transcellular transport. These nanoparticles have shown promising advancements in preclinical trials for the treatment of angiogenesis in ischemic stroke therapy.
To improve the permeability of the BBB, many strategies have been employed, including the utilization of BBB-targeting therapy-based nanoparticles, transcellular transport-based nanoparticles that undergo endocytosis, and biomimetic nanoparticles. These approaches aim to facilitate the penetration of a greater number of nanoparticles into the brain. Additional research is required to thoroughly examine the extended-term safety of this approach, given that an increased permeability of the BBB might heighten the potential for hemorrhagic transformation. In addition, enhancing the brain accumulation of nanoparticles by receptor-mediated transcytosis can be achieved by covalently conjugating or electrostatically interacting particular ligands with nanoparticles. Following a stroke, there is a notable upregulation of several receptors on the BBB, hence presenting novel prospects for the precise administration of nanomedicine.211–213 It is important to highlight that the use of targeted nanomedicine that has been changed with endogenous ligands may face competition from endogenous ligands present in the bloodstream during the process of crossing the BBB, resulting in a decrease in targeting effectiveness. Fortunately, there have been advancements in the development of antibodies that exhibit enhanced specificity towards receptors, hence rendering the interactions unaffected by endogenous ligands. Nevertheless, considering the extended circulation duration of nanoparticles, there is a possibility of heightened exposure to coagulation factors in the bloodstream, leading to an elevated risk of blood vessel blockages. This, in turn, can diminish the effectiveness of nanomedicine due to the acquisition of antigenic properties by plasma proteins after opsonization. The reticuloendothelial system has the potential to be significantly improved in terms of nanomedicine clearance.30 The necessity for validated methodologies to assess the cytotoxicity of nanomaterials arises from the fact that many types of nanomaterials have the potential to induce inflammation and generate free oxygen radicals. Hence, it is important to evaluate several crucial parameters, including the cell type, dose, and the impact of the biological environment on the physicochemical characteristics of nanomaterials. Additionally, careful consideration should be given to selecting the most suitable cytotoxic test.214
Simultaneously, the nanocarrier has been a significant focus of study due to its ability to carry medications across the blood-brain barrier and promote efficient drug release. Nanocarriers are highly valuable because of their unique targeting powers and prolonged circulation lifetime. Future study might prioritise investigating the inherent instability of liposomes, the possible toxicity associated with inorganic particles, and the intricate nature of polymer synthesis. Although several studies have validated the importance and efficacy of various drug delivery systems, their elimination from the body and potential adverse reactions still lack certainty. Moreover, given the complex characteristics of ischemic stroke, it is crucial for nanodelivery systems to prioritise the entire protection of the nervous system. Significantly, further investigation is need to examine a broader array of options, encompassing both preclinical and clinical phases.
Recent research have identified many therapeutic approaches for treating ischemic stroke by targeting nanotherapeutics that affect angiogenesis. The potential for these therapies to be applied in practice is reinforced by their great effectiveness in research conducted prior to clinical trials. Regrettably, none of the nanomedicines that have been examined have been effectively implemented in clinical settings thus far. Several issues impede the transfer from laboratory research to clinical use in the field, one of which is the constraints posed by preclinical stroke models. The MCAO animal stroke model is the most often utilised, although it is not suitable for clinically intricate situations that exhibit individual variations. Hence, it is imperative to create more suitable stroke models that accurately replicate the cellular and molecular processes involved in thrombosis and thrombolysis. Comorbidities pose an additional challenge in converting preclinical findings into practical applications. This problem presents a challenge when it comes to creating personalised treatments tailored to the patient’s specific ailment. In the coming years, we anticipate that nanotherapies specifically designed for Ischemic stroke will continue to advance. These treatments are expected to become more efficient and safer, which will make them more suitable for use in clinical settings. It should be emphasised that the nanoparticles formulations that are most efficient for delivering drugs to the brain nevertheless tend to collect in other parts of the body, such as the liver, spleen, kidney, and other organs and tissues, before being removed. Therefore, it is crucial to develop nanoformulations that are specifically activated to release the medicine after they have reached the brain, rather than doing so in other parts of the body.215 Future advancements in triggerable nanoformulations are anticipated to enhance the therapeutic application of nanoparticles in the field of regenerative medicine. Nanomedicines are still in the early stages of development and further comprehensive study is required to effectively transfer these pharmaceuticals into improving angiogenesis following brain ischemia. Additional inquiries should be undertaken to uncover the outcome of nanomedicines therapy targeting angiogenesis following stroke administration, as well as the potential adverse effects, in order to gain a deeper understanding of the transition from preclinical to clinical use.
Several types of nanoparticles to therapy of angiogenesis following stroke, including liposomes, inorganic nanoparticles, biomimetic nanoparticles, and polymeric nanoparticles, have been extensively studied. These particular types of nanoparticles have garnered significant attention due to their well-established manufacturing techniques, which has raised hopes for their potential translation into clinical applications. In recent times, there has been a growing interest in the development of biomimetic nanoparticles that utilize cell membranes or extracellular vesicles for the purpose of targeted drug administration in the context of angiogenesis following a stroke. The exceptional biocompatibility and safety, together with their intrinsic targeting properties, position them as a prominent area of research in the field of nanoparticles for the targeted therapy of angiogenesis following a stroke. This has the potential for significant advancements in stroke treatment.216 With advancements in carrier technology and a more comprehensive comprehension of pathogenic causes, nanoparticles have emerged as a promising avenue for exploring the therapy of angiogenesis following stroke.
Acknowledgments
This research was supported by the National Natural Science Foundation of China (82104147 to Guangtian Wang), the China Postdoctoral Special Grant Program (2022T150177 to Guangtian Wang), and the China Postdoctoral Program (2021M693833 to Guangtian Wang and 2020M681120 to Zhihui Li), the Innovative Scientific Research Grant Program of Harbin Medical University (2021-KYYWF-0272 to Guangtian Wang), and the and the Harbin Medical University Youth Fund (2023-KYYWF-0230 to Zhihui Li).
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Virani SS, Alonso A, Benjamin EJ, et al. American heart association council on, C. prevention statistics, S. stroke statistics, heart disease and stroke statistics-2020 update: a report from the American heart association. Circulation. 2020;141(9):e139–e596. doi:10.1161/CIR.0000000000000757
2. Hankey GJ. Stroke. Lancet. 2017;389(10069):641–654. doi:10.1016/S0140-6736(16)30962-X
3. Campbell BCV, De silva DA, Macleod MR, et al. Ischaemic stroke. Nat Rev Dis Primers. 2019;5(1):70. doi:10.1038/s41572-019-0118-8
4. Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344–e418. doi:10.1161/STR.0000000000000211
5. Betts KA, Hurley D, Song J, et al. Real-world outcomes of acute ischemic stroke treatment with intravenous recombinant tissue plasminogen activator. J Stroke Cerebrovasc Dis. 2017;26(9):1996–2003. doi:10.1016/j.jstrokecerebrovasdis.2017.06.010
6. Jin H, Bi R, Hu J, et al. Elevated serum lactate dehydrogenase predicts unfavorable outcomes After rt-PA thrombolysis in ischemic stroke patients. Front Neurol. 2022;13:816216. doi:10.3389/fneur.2022.816216
7. Liao J, Li Y, Luo Y, et al. Recent advances in targeted nanotherapies for ischemic stroke. Mol Pharm. 2022;19(9):3026–3041. doi:10.1021/acs.molpharmaceut.2c00383
8. Yang H, Luo Y, Hu H, et al. pH-Sensitive, cerebral vasculature-targeting hydroxyethyl starch functionalized nanoparticles for improved angiogenesis and neurological function recovery in ischemic stroke. Adv Healthc Mater. 2021;10(12):e2100028. doi:10.1002/adhm.202100028
9. Kaushal V, Schlichter LC. Mechanisms of microglia-mediated neurotoxicity in a new model of the stroke penumbra. J Neurosci. 2008;28(9):2221–2230. doi:10.1523/JNEUROSCI.5643-07.2008
10. Lo EH. A new penumbra: transitioning from injury into repair after stroke. Nat Med. 2008;14(5):497–500. doi:10.1038/nm1735
11. Hermann DM, Zechariah A. Implications of vascular endothelial growth factor for postischemic neurovascular remodeling. J Cereb Blood Flow Metab. 2009;29(10):1620–1643. doi:10.1038/jcbfm.2009.100
12. Snapyan M, Lemasson MS, Brill M, et al. Saghatelyan, Vasculature guides migrating neuronal precursors in the adult mammalian forebrain via brain-derived neurotrophic factor signaling. J Neurosci. 2009;29(13):4172–4188. doi:10.1523/JNEUROSCI.4956-08.2009
13. Teng H, Zhang ZG, Wang L, et al. Coupling of angiogenesis and neurogenesis in cultured endothelial cells and neural progenitor cells after stroke. J Cereb Blood Flow Metab. 2008;28(4):764–771. doi:10.1038/sj.jcbfm.9600573
14. Yang Y, Torbey MT. Angiogenesis and blood-brain barrier permeability in vascular remodeling after stroke. Curr Neuropharmacol. 2020;18(12):1250–1265. doi:10.2174/1570159X18666200720173316
15. Xie C, Liao J, Zhang N, et al. Advanced nano drug delivery systems for neuroprotection against ischemic stroke. Chin. Chem. Lett. 2024;35(2):109149. doi:10.1016/j.cclet.2023.109149
16. Yoo SY, Kwon SM. Angiogenesis and its therapeutic opportunities. Mediators Inflamm. 2013;2013:127170. doi:10.1155/2013/127170
17. Carmeliet P, Jain RK. Molecular mechanisms and clinical applications of angiogenesis. Nature. 2011;473(7347):298–307. doi:10.1038/nature10144
18. Adams RH, Alitalo K. Molecular regulation of angiogenesis and lymphangiogenesis. Nat Rev Mol Cell Biol. 2007;8(6):464–478. doi:10.1038/nrm2183
19. Freedman SB, Isner JM. Therapeutic angiogenesis for ischemic cardiovascular disease. J Mol Cell Cardiol. 2001;33(3):379–393. doi:10.1006/jmcc.2000.1329
20. Ribatti D, Conconi MT, Nussdorfer GG. Nonclassic endogenous novel [corrected] regulators of angiogenesis. Pharmacol Rev. 2007;59(2):185–205. doi:10.1124/pr.59.2.3
21. Zhao L, Johnson T, Liu D. Therapeutic angiogenesis of adipose-derived stem cells for ischemic diseases. Stem Cell Res Ther. 2017;8(1):125. doi:10.1186/s13287-017-0578-2
22. Wang AZ, Langer R, Farokhzad OC. Nanoparticle delivery of cancer drugs. Annu Rev Med. 2012;63:185–198. doi:10.1146/annurev-med-040210-162544
23. Farokhzad OC, Langer R. Impact of nanotechnology on drug delivery. ACS Nano. 2009;3(1):16–20. doi:10.1021/nn900002m
24. Kaviarasi S, Yuba E, Harada A, Krishnan UM. Emerging paradigms in nanotechnology for imaging and treatment of cerebral ischemia. J Control Release. 2019;300:22–45. doi:10.1016/j.jconrel.2019.02.031
25. Knowland D, Arac A, Sekiguchi KJ, et al. Stepwise recruitment of transcellular and paracellular pathways underlies blood-brain barrier breakdown in stroke. Neuron. 2014;82(3):603–617. doi:10.1016/j.neuron.2014.03.003
26. Dong X, Gao J, Su Y, Wang Z. Nanomedicine for ischemic stroke. Int J Mol Sci. 2020;21(20):7600. doi:10.3390/ijms21207600
27. Pulicherla KK, Verma MK. Targeting therapeutics across the blood brain barrier (BBB), prerequisite towards thrombolytic therapy for cerebrovascular disorders-an overview and advancements. AAPS Pharm Sci Tech. 2015;16(2):223–233. doi:10.1208/s12249-015-0287-z
28. Chik MW, Hussain Z, Zulkefeli M, et al. Polymer-wrapped single-walled carbon nanotubes: a transformation toward better applications in healthcare. Drug Deliv Transl Res. 2019;9(2):578–594. doi:10.1007/s13346-018-0505-9
29. Panagiotou S, Saha S. Therapeutic benefits of nanoparticles in stroke. Front Neurosci. 2015;9:182. doi:10.3389/fnins.2015.00182
30. Sarmah D, Saraf J, Kaur H, et al. Stroke management: an emerging role of nanotechnology. Micromachines. 2017;8(9):1.
31. Kyle S, Saha S. Nanotechnology for the detection and therapy of stroke. Adv Healthc Mater. 2014;3(11):1703–1720. doi:10.1002/adhm.201400009
32. Shen J, Zhao Z, Shang W, et al. Fabrication and evaluation a transferrin receptor targeting nano-drug carrier for cerebral infarction treatment. Artif Cells Nanomed Biotechnol. 2019;47(1):192–200. doi:10.1080/21691401.2018.1548471
33. Carenza E, Jordan O, Martinez-San Segundo P, et al. Encapsulation of VEGF(165) into magnetic PLGA nanocapsules for potential local delivery and bioactivity in human brain endothelial cells. J Mater Chem B. 2015;3(12):2538–2544. doi:10.1039/C4TB01895H
34. Deng L, Zhang F, Wu Y, et al. RGD-modified nanocarrier-mediated targeted delivery of HIF-1alpha-AA Plasmid DNA to cerebrovascular endothelial cells for ischemic stroke treatment. ACS Biomater Sci Eng. 2019;5(11):6254–6264. doi:10.1021/acsbiomaterials.9b01362
35. Wang C, Lin G, Luan Y, et al. HIF-prolyl hydroxylase 2 silencing using siRNA delivered by MRI-visible nanoparticles improves therapy efficacy of transplanted EPCs for ischemic stroke. Biomaterials. 2019;197:229–243. doi:10.1016/j.biomaterials.2018.05.053
36. Shen J, Zhao Z, Shang W, et al. Fabrication of a nano polymer wrapping Meg3 ShRNA plasmid for the treatment of cerebral infarction. Artif Cells Nanomed Biotechnol. 2018;46(sup2):894–903. doi:10.1080/21691401.2018.1471483
37. Ferreira R, Fonseca MC, Santos T, et al. Retinoic acid-loaded polymeric nanoparticles enhance vascular regulation of neural stem cell survival and differentiation after ischaemia. Nanoscale. 2016;8(15):8126–8137. doi:10.1039/C5NR09077F
38. Petro M, Jaffer H, Yang J, Kabu S, Morris VB, Labhasetwar V. Tissue plasminogen activator followed by antioxidant-loaded nanoparticle delivery promotes activation/mobilization of progenitor cells in infarcted rat brain. Biomaterials. 2016;81:169–180. doi:10.1016/j.biomaterials.2015.12.009
39. Lu X, Dong J, Zheng D, Li X, Ding D, Xu H. Reperfusion combined with intraarterial administration of resveratrol-loaded nanoparticles improved cerebral ischemia-reperfusion injury in rats. Nanomedicine. 2020;28:102208. doi:10.1016/j.nano.2020.102208
40. Li X, Han Z, Wang T, et al. Cerium oxide nanoparticles with antioxidative neurorestoration for ischemic stroke. Biomaterials. 2022;291:121904. doi:10.1016/j.biomaterials.2022.121904
41. Wang J, Su Q, Lv Q, et al. Oxygen-generating cyanobacteria powered by upconversion-nanoparticles-converted near-infrared light for ischemic stroke treatment. Nano Lett. 2021;21(11):4654–4665. doi:10.1021/acs.nanolett.1c00719
42. Li Y, Zhang M, Li S, et al. Selective ischemic-hemisphere targeting Ginkgolide B liposomes with improved solubility and therapeutic efficacy for cerebral ischemia-reperfusion injury. Asian J Pharm Sci. 2023;18(2):100783. doi:10.1016/j.ajps.2023.100783
43. Xia Y, Ling X, Hu G, et al. Small extracellular vesicles secreted by human iPSC-derived MSC enhance angiogenesis through inhibiting STAT3-dependent autophagy in ischemic stroke. Stem Cell Res Ther. 2020;11(1):313. doi:10.1186/s13287-020-01834-0
44. Gregorius J, Wang C, Stambouli O, et al. Small extracellular vesicles obtained from hypoxic mesenchymal stromal cells have unique characteristics that promote cerebral angiogenesis, brain remodeling and neurological recovery after focal cerebral ischemia in mice. Basic Res Cardiol. 2021;116(1):40. doi:10.1007/s00395-021-00881-9
45. Mohamud Yusuf A, Hagemann N, Zhang X, et al. Acid sphingomyelinase deactivation post-ischemia promotes brain angiogenesis and remodeling by small extracellular vesicles. Basic Res Cardiol. 2022;117(1):43. doi:10.1007/s00395-022-00950-7
46. Zhang L, Wei W, Ai X, et al. Extracellular vesicles from hypoxia-preconditioned microglia promote angiogenesis and repress apoptosis in stroke mice via the TGF-beta/Smad2/3 pathway. Cell Death Dis. 2021;12(11):1068. doi:10.1038/s41419-021-04363-7
47. Wang C, Yang X, Jiang Y, et al. Targeted delivery of fat extract by platelet membrane-cloaked nanocarriers for the treatment of ischemic stroke. J Nanobiotechnology. 2022;20(1):249. doi:10.1186/s12951-022-01461-2
48. Katas H, Wen CY, Siddique MI, Hussain Z, Mohd Fadhil FH. Thermoresponsive curcumin/DsiRNA nanoparticle gels for the treatment of diabetic wounds: synthesis and drug release. Ther Deliv. 2017;8(3):137–150. doi:10.4155/tde-2016-0075
49. Hussain Z, Katas H, Yan SL, Jamaludin D. Efficient colonic delivery of DsiRNA by pectin-coated polyelectrolyte complex nanoparticles: preparation, characterization and improved gastric survivability. Curr Drug Deliv. 2017;14(7):1016–1027. doi:10.2174/1567201814666170224142446
50. Ei Thu H, Hussain Z, Shuid AN. New insight in improving therapeutic efficacy of antipsychotic agents: an overview of improved in vitro and in vivo performance, efficacy upgradation and future prospects. Curr Drug Targets. 2018;19(8):865–876. doi:10.2174/1389450117666161125174625
51. Zia MA, Sohail M, Minhas M, et al. HEMA based pH-sensitive semi IPN microgels for oral delivery; a rationale approach for ketoprofen. Drug Dev Ind Pharm. 2020;46(2):272–282. doi:10.1080/03639045.2020.1716378
52. Chen W, Jiang L, Hu Y, et al. Nanomedicines, an emerging therapeutic regimen for treatment of ischemic cerebral stroke: a review. J Control Release. 2021;340:342–360. doi:10.1016/j.jconrel.2021.10.020
53. Masserini M. Nanoparticles for brain drug delivery. ISRN Biochem. 2013;2013:238428.
54. Chen C, Mu XY, Zhou Y, et al. Ginsenoside Rg1 enhances the resistance of hematopoietic stem/progenitor cells to radiation-induced aging in mice. Acta Pharmacol Sin. 2014;35(1):143–150. doi:10.1038/aps.2013.136
55. Wang J, Li D, Hou J, Lei H. Protective effects of geniposide and ginsenoside Rg1 combination treatment on rats following cerebral ischemia are mediated via microglial microRNA‑155‑5p inhibition. Mol Med Rep. 2018;17(2):3186–3193. doi:10.3892/mmr.2017.8221
56. Xie CL, Li JH, Wang WW, Zheng GQ, Wang LX. Neuroprotective effect of ginsenoside-Rg1 on cerebral ischemia/reperfusion injury in rats by downregulating protease-activated receptor-1 expression. Life Sci. 2015;121:145–151. doi:10.1016/j.lfs.2014.12.002
57. Li Y-B, Wang Y, Tang J-P, Chen D, Wang S-L. Neuroprotective effects of ginsenoside Rg1-induced neural stem cell transplantation on hypoxic-ischemic encephalopathy. Neural Regen Res. 2015;10(5):753–759. doi:10.4103/1673-5374.156971
58. Shen HH. Core Concept: circumventing the blood-brain barrier. Proc Natl Acad Sci U S A. 2017;114(43):11261–11263. doi:10.1073/pnas.1716187114
59. Nogueira-Librelotto DR, Codevilla CF, Farooqi A, Rolim CM. Transferrin-conjugated nanocarriers as active-targeted drug delivery platforms for cancer therapy. Curr Pharm Des. 2017;23(3):454–466. doi:10.2174/1381612822666161026162347
60. Han L, Li J, Huang S, et al. Peptide-conjugated polyamidoamine dendrimer as a nanoscale tumor-targeted T1 magnetic resonance imaging contrast agent. Biomaterials. 2011;32(11):2989–2998. doi:10.1016/j.biomaterials.2011.01.005
61. Zhang L, Wang T, Li Q, et al. Fabrication of novel vesicles of triptolide for antirheumatoid activity with reduced toxicity in vitro and in vivo. Int J Nanomed. 2016;11:2663–2673. doi:10.2147/IJN.S104593
62. Geng X, Ye H, Feng Z, et al. Synthesis and characterization of cisplatin-loaded, EGFR-targeted biopolymer and in vitro evaluation for targeted delivery. J Biomed Mater Res A. 2012;100(10):2839–2848. doi:10.1002/jbm.a.34207
63. Zhang L, Chang J, Zhao Y, et al. Fabrication of a triptolide-loaded and poly-gamma-glutamic acid-based amphiphilic nanoparticle for the treatment of rheumatoid arthritis. Int J Nanomed. 2018;13:2051–2064. doi:10.2147/IJN.S151233
64. Carenza E, Barcelo V, Morancho A, et al. In vitro angiogenic performance and in vivo brain targeting of magnetized endothelial progenitor cells for neurorepair therapies. Nanomedicine. 2014;10(1):225–234. doi:10.1016/j.nano.2013.06.005
65. Bible E, Qutachi O, Chau DY, Alexander MR, Shakesheff KM, Modo M. Neo-vascularization of the stroke cavity by implantation of human neural stem cells on VEGF-releasing PLGA microparticles. Biomaterials. 2012;33(30):7435–7446. doi:10.1016/j.biomaterials.2012.06.085
66. Formiga FR, Pelacho B, Garbayo E, et al. Sustained release of VEGF through PLGA microparticles improves vasculogenesis and tissue remodeling in an acute myocardial ischemia-reperfusion model. J Control Release. 2010;147(1):30–37. doi:10.1016/j.jconrel.2010.07.097
67. Golub JS, Kim YT, Duvall CL, et al. Sustained VEGF delivery via PLGA nanoparticles promotes vascular growth. Am J Physiol Heart Circ Physiol. 2010;298(6):H1959–65. doi:10.1152/ajpheart.00199.2009
68. Rhim T, Lee DY, Lee M. Drug delivery systems for the treatment of ischemic stroke. Pharm Res. 2013;30(10):2429–2444. doi:10.1007/s11095-012-0959-2
69. Des Rieux A, Ucakar BP, Mupendwa B, et al. 3D systems delivering VEGF to promote angiogenesis for tissue engineering. J Control Release. 2011;150(3):272–278. doi:10.1016/j.jconrel.2010.11.028
70. Borselli C, Ungaro F, Oliviero O, et al. Bioactivation of collagen matrices through sustained VEGF release from PLGA microspheres. J Biomed Mater Res A. 2010;92(1):94–102. doi:10.1002/jbm.a.32332
71. Kim J, Cao L, Shvartsman D, Silva EA, Mooney DJ. Targeted delivery of nanoparticles to ischemic muscle for imaging and therapeutic angiogenesis. Nano Lett. 2011;11(2):694–700. doi:10.1021/nl103812a
72. Liu X, Kaminski MD, Chen H, Torno M, Taylor L, Rosengart AJ. Synthesis and characterization of highly-magnetic biodegradable poly(d,l-lactide-co-glycolide) nanospheres. J Control Release. 2007;119(1):52–58. doi:10.1016/j.jconrel.2006.11.031
73. Okassa LN, Marchais H, Douziech-Eyrolles L, et al. Optimization of iron oxide nanoparticles encapsulation within poly(d,l-lactide-co-glycolide) sub-micron particles. Eur J Pharm Biopharm. 2007;67(1):31–38. doi:10.1016/j.ejpb.2006.12.020
74. Khan M, Dhammu TS, Matsuda F, et al. Promoting endothelial function by S-nitrosoglutathione through the HIF-1alpha/VEGF pathway stimulates neurorepair and functional recovery following experimental stroke in rats. Drug Des Devel Ther. 2015;9:2233–2247. doi:10.2147/DDDT.S77115
75. Doeppner TR, Mlynarczuk-Bialy I, Kuckelkorn U, et al. The novel proteasome inhibitor BSc2118 protects against cerebral ischaemia through HIF1A accumulation and enhanced angioneurogenesis. Brain. 2012;135(Pt 11):3282–3297. doi:10.1093/brain/aws269
76. Zhong Q, Zhou Y, Ye W, Cai T, Zhang X, Deng DY. Hypoxia-inducible factor 1-alpha-AA-modified bone marrow stem cells protect PC12 cells from hypoxia-induced apoptosis, partially through VEGF/PI3K/Akt/FoxO1 pathway. Stem Cells Dev. 2012;21(14):2703–2717. doi:10.1089/scd.2011.0604
77. Bharadwaj VN, Nguyen DT, Kodibagkar VD, Stabenfeldt SE. Nanoparticle-based therapeutics for brain injury. Adv Healthc Mater. 2018;7(1). doi:10.1002/adhm.201700668
78. Berra E, Benizri E, Ginouves A, et al. HIF prolyl-hydroxylase 2 is the key oxygen sensor setting low steady-state levels of HIF-1alpha in normoxia. EMBO J. 2003;22(16):4082–4090. doi:10.1093/emboj/cdg392
79. Wu S, Nishiyama N, Kano MR, et al. Enhancement of angiogenesis through stabilization of hypoxia-inducible factor-1 by silencing prolyl hydroxylase domain-2 gene. Mol Ther. 2008;16(7):1227–1234. doi:10.1038/mt.2008.90
80. Jaakkola P, Mole DR, Tian YM, et al. Targeting of HIF-alpha to the von Hippel-Lindau ubiquitylation complex by O2-regulated prolyl hydroxylation. Science. 2001;292(5516):468–472. doi:10.1126/science.1059796
81. Oh YK, Park TG. siRNA delivery systems for cancer treatment. Adv Drug Deliv Rev. 2009;61(10):850–862. doi:10.1016/j.addr.2009.04.018
82. Hong CA, Nam YS. Functional nanostructures for effective delivery of small interfering RNA therapeutics. Theranostics. 2014;4(12):1211–1232. doi:10.7150/thno.8491
83. Lin G, Zhu W, Yang L, et al. Delivery of siRNA by MRI-visible nanovehicles to overcome drug resistance in MCF-7/ADR human breast cancer cells. Biomaterials. 2014;35(35):9495–9507. doi:10.1016/j.biomaterials.2014.07.049
84. Liu G, Xie J, Zhang F, et al. N-Alkyl-PEI-functionalized iron oxide nanoclusters for efficient siRNA delivery. Small. 2011;7(19):2742–2749. doi:10.1002/smll.201100825
85. Yan B, Yao J, Liu JY, et al. lncRNA-MIAT regulates microvascular dysfunction by functioning as a competing endogenous RNA. Circ Res. 2015;116(7):1143–1156. doi:10.1161/CIRCRESAHA.116.305510
86. Yan H, Yuan J, Gao L, et al. Long noncoding RNA MEG3 activation of p53 mediates ischemic neuronal death in stroke. Neuroscience. 2016;337:191–199. doi:10.1016/j.neuroscience.2016.09.017
87. Zhou Y, Cheunsuchon P, Nakayama Y, et al. Activation of paternally expressed genes and perinatal death caused by deletion of the Gtl2 gene. Development. 2010;137(16):2643–2652. doi:10.1242/dev.045724
88. Gordon FE, Nutt CL, Cheunsuchon P, et al. Increased expression of angiogenic genes in the brains of mouse meg3-null embryos. Endocrinology. 2010;151(6):2443–2452. doi:10.1210/en.2009-1151
89. Su W, Xie W, Shang Q, Su B. The Long Noncoding RNA MEG3 Is Downregulated and Inversely Associated with VEGF Levels in Osteoarthritis. Biomed Res Int. 2015;2015:356893. doi:10.1155/2015/356893
90. He Y, Luo Y, Liang B, Ye L, Lu G, He W. Potential applications of MEG3 in cancer diagnosis and prognosis. Oncotarget. 2017;8(42):73282–73295. doi:10.18632/oncotarget.19931
91. Hui F, Nguyen CTO, He Z, et al. Retinal and cortical blood flow dynamics following systemic blood-neural barrier disruption. Front Neurosci. 2017;11:568. doi:10.3389/fnins.2017.00568
92. Liu Z, Zhang L, He Q, et al. Effect of Baicalin-loaded PEGylated cationic solid lipid nanoparticles modified by OX26 antibody on regulating the levels of baicalin and amino acids during cerebral ischemia-reperfusion in rats. Int J Pharm. 2015;489(1–2):131–138. doi:10.1016/j.ijpharm.2015.04.049
93. Peng SF, Tseng MT, Ho YC, Wei MC, Liao ZX, Sung HW. Mechanisms of cellular uptake and intracellular trafficking with chitosan/DNA/poly(gamma-glutamic acid) complexes as a gene delivery vector. Biomaterials. 2011;32(1):239–248. doi:10.1016/j.biomaterials.2010.08.081
94. Deng J, Wen Y, Wang C, et al. Efficient intracellular gene delivery using the formulation composed of poly (L-glutamic acid) grafted polyethylenimine and histone. Pharm Res. 2011;28(4):812–826. doi:10.1007/s11095-010-0335-z
95. Sawada M, Matsumoto M, Sawamoto K. Vascular regulation of adult neurogenesis under physiological and pathological conditions. Front Neurosci. 2014;8:53. doi:10.3389/fnins.2014.00053
96. Maden M. Retinoic acid in the development, regeneration and maintenance of the nervous system. Nat Rev Neurosci. 2007;8(10):755–765. doi:10.1038/nrn2212
97. Saito A, Sugawara A, Uruno A, et al. All-trans retinoic acid induces in vitro angiogenesis via retinoic acid receptor: possible involvement of paracrine effects of endogenous vascular endothelial growth factor signaling. Endocrinology. 2007;148(3):1412–1423. doi:10.1210/en.2006-0900
98. Jin Y, Raviv N, Barnett A, Bambakidis NC, Filichia E, Luo Y. The shh signaling pathway is upregulated in multiple cell types in cortical ischemia and influences the outcome of stroke in an animal model. PLoS One. 2015;10(4):e0124657. doi:10.1371/journal.pone.0124657
99. Zhang X, Zhou Y, Li H, et al. Intravenous administration of DPSCs and BDNF improves neurological performance in rats with focal cerebral ischemia. Int J Mol Med. 2018;41(6):3185–3194. doi:10.3892/ijmm.2018.3517
100. Zhang ZG, Zhang L, Tsang W, et al. Correlation of VEGF and angiopoietin expression with disruption of blood-brain barrier and angiogenesis after focal cerebral ischemia. J Cereb Blood Flow Metab. 2002;22(4):379–392. doi:10.1097/00004647-200204000-00002
101. Li S, Nih LR, Bachman H, et al. Hydrogels with precisely controlled integrin activation dictate vascular patterning and permeability. Nat Mater. 2017;16(9):953–961. doi:10.1038/nmat4954
102. Nih LR, Gojgini ST, Carmichael S, Segura T. Dual-function injectable angiogenic biomaterial for the repair of brain tissue following stroke. Nat Mater. 2018;17(7):642–651. doi:10.1038/s41563-018-0083-8
103. Campbell ID, Humphries MJ. Integrin structure, activation, and interactions. Cold Spring Harb Perspect Biol. 2011;3(3):a004994–a004994. doi:10.1101/cshperspect.a004994
104. Sun J, Yu L, Huang S, Lai X, Milner R, Li L. Vascular expression of angiopoietin1, alpha5beta1 integrin and tight junction proteins is tightly regulated during vascular remodeling in the post-ischemic brain. Neuroscience. 2017;362:248–256. doi:10.1016/j.neuroscience.2017.08.040
105. Feng Y, Mrksich M. The synergy peptide PHSRN and the adhesion peptide RGD mediate cell adhesion through a common mechanism. Biochemistry. 2004;43(50):15811–15821.
106. Wu CC, Wang LC, Su YT, Wei WY, Tsai KJ. Synthetic alpha5beta1 integrin ligand PHSRN is proangiogenic and neuroprotective in cerebral ischemic stroke. Biomaterials. 2018;185:142–154. doi:10.1016/j.biomaterials.2018.09.014
107. Cui W, Liu R, Jin H, et al. pH gradient difference around ischemic brain tissue can serve as a trigger for delivering polyethylene glycol-conjugated urokinase nanogels. J Control Release. 2016;225:53–63. doi:10.1016/j.jconrel.2016.01.028
108. Luo Y, Yang H, Zhou YF, Hu B. Dual and multi-targeted nanoparticles for site-specific brain drug delivery. J Control Release. 2020;317:195–215. doi:10.1016/j.jconrel.2019.11.037
109. Cheng R, Meng F, Deng C, Klok HA, Zhong Z. Dual and multi-stimuli responsive polymeric nanoparticles for programmed site-specific drug delivery. Biomaterials. 2013;34(14):3647–3657. doi:10.1016/j.biomaterials.2013.01.084
110. Hu H, Li Y, Zhou Q, et al. Redox-sensitive hydroxyethyl starch-doxorubicin conjugate for tumor targeted drug delivery. ACS Appl Mater Interfaces. 2016;8(45):30833–30844. doi:10.1021/acsami.6b11932
111. Hu H, Xiao C, Wu H, et al. Nanocolloidosomes with selective drug release for active tumor-targeted imaging-guided photothermal/chemo combination therapy. ACS Appl Mater Interfaces. 2017;9(48):42225–42238. doi:10.1021/acsami.7b14796
112. Esquiva G, Grayston A, Rosell A. Revascularization and endothelial progenitor cells in stroke. Am J Physiol Cell Physiol. 2018;315(5):C664–C674. doi:10.1152/ajpcell.00200.2018
113. Aziz A, Haywood NJ, Cordell PA, et al. Insulin like growth factor-binding protein-1 improves vascular endothelial repair in male mice in the setting of insulin resistance. Endocrinology. 2018;159(2):696–709. doi:10.1210/en.2017-00572
114. Wang H, Yin YG, Huang H, et al. Transplantation of EPCs overexpressing PDGFR-beta promotes vascular repair in the early phase after vascular injury. BMC Cardiovasc Disord. 2016;16(1):179. doi:10.1186/s12872-016-0353-9
115. Wang H, Yin Y, Li W, et al. Over-expression of PDGFR-beta promotes PDGF-induced proliferation, migration, and angiogenesis of EPCs through PI3K/Akt signaling pathway. PLoS One. 2012;7(2):e30503. doi:10.1371/journal.pone.0030503
116. Seto SW, Chang D, Jenkins A, Bensoussan A, Kiat H. Angiogenesis in ischemic stroke and angiogenic effects of Chinese herbal medicine. J Clin Med. 2016;5(6):56. doi:10.3390/jcm5060056
117. Ergul A, Alhusban A, Fagan SC. Angiogenesis: a harmonized target for recovery after stroke. Stroke. 2012;43(8):2270–2274. doi:10.1161/STROKEAHA.111.642710
118. Manoonkitiwongsa PS, Jackson-Friedman C, McMillan PJ, Schultz RL, Lyden PD. Angiogenesis after stroke is correlated with increased numbers of macrophages: the clean-up hypothesis. J Cereb Blood Flow Metab. 2001;21(10):1223–1231. doi:10.1097/00004647-200110000-00011
119. Fang W, Zhai X, Han D, et al. CCR2-dependent monocytes/macrophages exacerbate acute brain injury but promote functional recovery after ischemic stroke in mice. Theranostics. 2018;8(13):3530–3543. doi:10.7150/thno.24475
120. Zong X, Li Y, Liu C, et al. Theta-burst transcranial magnetic stimulation promotes stroke recovery by vascular protection and neovascularization. Theranostics. 2020;10(26):12090–12110. doi:10.7150/thno.51573
121. Jickling GC, Liu D, Stamova B, et al. Hemorrhagic transformation after ischemic stroke in animals and humans. J Cereb Blood Flow Metab. 2014;34(2):185–199. doi:10.1038/jcbfm.2013.203
122. Villaran RF, de Pablos RM, Arguelles S, et al. The intranigral injection of tissue plasminogen activator induced blood-brain barrier disruption, inflammatory process and degeneration of the dopaminergic system of the rat. Neurotoxicology. 2009;30(3):403–413. doi:10.1016/j.neuro.2009.02.011
123. Wahlgren N, Ahmed N, Davalos A, et al. Thrombolysis with alteplase 3-4.5 h after acute ischaemic stroke (SITS-ISTR): an observational study. Lancet. 2008;372(9646):1303–1309. doi:10.1016/S0140-6736(08)61339-2
124. Moskowitz MA, Lo EH, Iadecola C. The science of stroke: mechanisms in search of treatments. Neuron. 2010;67(2):181–198. doi:10.1016/j.neuron.2010.07.002
125. Sun T, Jiang C. Stimuli-responsive drug delivery systems triggered by intracellular or subcellular microenvironments. Adv Drug Deliv Rev. 2023;196:114773. doi:10.1016/j.addr.2023.114773
126. Zhu W, Huang L, Li Y, et al. Exosomes derived from human bone marrow mesenchymal stem cells promote tumor growth in vivo. Cancer Lett. 2012;315(1):28–37. doi:10.1016/j.canlet.2011.10.002
127. Urban N, Guillemot F. Neurogenesis in the embryonic and adult brain: same regulators, different roles. Front Cell Neurosci. 2014;8:396. doi:10.3389/fncel.2014.00396
128. Dibajnia P, Morshead CM. Role of neural precursor cells in promoting repair following stroke. Acta Pharmacol Sin. 2013;34(1):78–90. doi:10.1038/aps.2012.107
129. Huang TT, Zou Y, Corniola R. Oxidative stress and adult neurogenesis--effects of radiation and superoxide dismutase deficiency. Semin Cell Dev Biol. 2012;23(7):738–744. doi:10.1016/j.semcdb.2012.04.003
130. Mizuma A, Yenari MA. Anti-inflammatory targets for the treatment of reperfusion injury in stroke. Front Neurol. 2017;8:467. doi:10.3389/fneur.2017.00467
131. Chelluboina B, Klopfenstein JD, Gujrati M, Rao JS, Veeravalli KK. Temporal regulation of apoptotic and anti-apoptotic molecules after middle cerebral artery occlusion followed by reperfusion. Mol Neurobiol. 2014;49(1):50–65. doi:10.1007/s12035-013-8486-7
132. Carta G, Poddighe L, Serra MP, et al. Preventive effects of resveratrol on endocannabinoid system and synaptic protein modifications in rat cerebral cortex challenged by bilateral common carotid artery occlusion and reperfusion. Int J Mol Sci. 2018;19(2):426. doi:10.3390/ijms19020426
133. Fonseca-Santos B, Satake CY, Calixto GMF, Dos Santos AM, Chorilli M. Trans-resveratrol-loaded nonionic lamellar liquid-crystalline systems: structural, rheological, mechanical, textural, and bioadhesive characterization and evaluation of in vivo anti-inflammatory activity. Int J Nanomed. 2017;12:6883–6893. doi:10.2147/IJN.S138629
134. Lu X, Xu H, Sun B, Zhu Z, Zheng D, Li X. Enhanced neuroprotective effects of resveratrol delivered by nanoparticles on hydrogen peroxide-induced oxidative stress in rat cortical cell culture. Mol Pharm. 2013;10(5):2045–2053. doi:10.1021/mp400056c
135. Barui AK, Jhelum P, Nethi SK, et al. Potential therapeutic application of zinc oxide nanoflowers in the cerebral ischemia rat model through neuritogenic and neuroprotective properties. Bioconjug Chem. 2020;31(3):895–906. doi:10.1021/acs.bioconjchem.0c00030
136. Kim CK, Kim T, Choi IY, et al. Ceria nanoparticles that can protect against ischemic stroke. Angew Chem Int Ed Engl. 2012;51(44):11039–11043. doi:10.1002/anie.201203780
137. Liao J, Li Y, Fan L, et al. Bioactive ceria nanoenzymes target mitochondria in reperfusion injury to treat ischemic stroke. ACS Nano. 2024;2014:1.
138. He L, Huang G, Liu H, Sang C, Liu X, Chen T. Highly bioactive zeolitic imidazolate framework-8-capped nanotherapeutics for efficient reversal of reperfusion-induced injury in ischemic stroke. Sci Adv. 2020;6(12):eaay9751. doi:10.1126/sciadv.aay9751
139. Wang S, Ma F, Huang L, et al. Dl-3-n-Butylphthalide (NBP): a promising therapeutic agent for ischemic stroke. CNS Neurol Disord Drug Targets. 2018;17(5):338–347. doi:10.2174/1871527317666180612125843
140. Qin C, Zhou P, Wang L, et al. Dl-3-N-butylphthalide attenuates ischemic reperfusion injury by improving the function of cerebral artery and circulation. J Cereb Blood Flow Metab. 2019;39(10):2011–2021. doi:10.1177/0271678X18776833
141. Yang CS, Guo A, Li Y, Shi K, Shi FD, Li M. Dl-3-n-butylphthalide reduces neurovascular inflammation and ischemic brain injury in mice. Aging Dis. 2019;10(5):964–976. doi:10.14336/AD.2019.0608
142. Yang LC, Li J, Xu SF, et al. L-3-n-butylphthalide promotes neurogenesis and neuroplasticity in cerebral ischemic rats. CNS Neurosci Ther. 2015;21(9):733–741. doi:10.1111/cns.12438
143. Liu S, Shi H, Liu W, Furuichi T, Timmins GS, Liu KJ. Interstitial pO2 in ischemic penumbra and core are differentially affected following transient focal cerebral ischemia in rats. J Cereb Blood Flow Metab. 2004;24(3):343–349. doi:10.1097/01.WCB.0000110047.43905.01
144. Atsumi S, Higashide W, Liao JC. Direct photosynthetic recycling of carbon dioxide to isobutyraldehyde. Nat Biotechnol. 2009;27(12):1177–1180. doi:10.1038/nbt.1586
145. Xu Y, Ma P, Shah P, Rokas A, Liu Y, Johnson CH. Non-optimal codon usage is a mechanism to achieve circadian clock conditionality. Nature. 2013;495(7439):116–120. doi:10.1038/nature11942
146. Cohen JE, Goldstone AB, Paulsen MJ, et al. An innovative biologic system for photon-powered myocardium in the ischemic heart. Sci Adv. 2017;3(6):e1603078. doi:10.1126/sciadv.1603078
147. Qiao Y, Yang F, Xie T, et al. Engineered algae: a novel oxygen-generating system for effective treatment of hypoxic cancer. Sci Adv. 2020;6(21):eaba5996. doi:10.1126/sciadv.aba5996
148. Weissleder R. A clearer vision for in vivo imaging. Nat Biotechnol. 2001;19(4):316–317. doi:10.1038/86684
149. Liu J, Pan L, Shang C, et al. A highly sensitive and selective nanosensor for near-infrared potassium imaging. Sci Adv. 2020;6(16):eaax9757. doi:10.1126/sciadv.aax9757
150. Byrdin M, Jordan P, Krauss N, Fromme P, Stehlik D, Schlodder E. Light harvesting in photosystem I: modeling based on the 2.5-A structure of photosystem I from Synechococcus elongatus. Biophys J. 2002;83(1):433–457. doi:10.1016/S0006-3495(02)75181-3
151. Dau H, Zaharieva I. Principles, efficiency, and blueprint character of solar-energy conversion in photosynthetic water oxidation. Acc Chem Res. 2009;42(12):1861–1870. doi:10.1021/ar900225y
152. Wang F, Deng R, Wang J, et al. Tuning upconversion through energy migration in core-shell nanoparticles. Nat Mater. 2011;10(12):968–973. doi:10.1038/nmat3149
153. Wang J, Wang F, Wang C, Liu Z, Liu X. Single-band upconversion emission in lanthanide-doped KMnF3 nanocrystals. Angew Chem Int Ed Engl. 2011;50(44):10369–10372. doi:10.1002/anie.201104192
154. Allen TM, Cullis PR. Liposomal drug delivery systems: from concept to clinical applications. Adv Drug Deliv Rev. 2013;65(1):36–48. doi:10.1016/j.addr.2012.09.037
155. Al-Ahmady ZS, Jasim D, Ahmad SS, et al. Selective liposomal transport through blood brain barrier disruption in ischemic stroke reveals two distinct therapeutic opportunities. ACS Nano. 2019;13(11):12470–12486. doi:10.1021/acsnano.9b01808
156. Terstappen GC, Meyer AH, Bell RD, Zhang W. Strategies for delivering therapeutics across the blood-brain barrier. Nat Rev Drug Discov. 2021;20(5):362–383. doi:10.1038/s41573-021-00139-y
157. Li C, Liu K, Liu S, Aerqin Q, Wu X. Role of ginkgolides in the inflammatory immune response of neurological diseases: a review of current literatures. Front Syst Neurosci. 2020;14:45. doi:10.3389/fnsys.2020.00045
158. Wei H, Sun T, Tian Y, Wang K. Ginkgolide B Modulates BDNF expression in acute ischemic stroke. J Korean Neurosurg Soc. 2017;60(4):391–396. doi:10.3340/jkns.2016.1010.018
159. Zheng PD, Mungur R, Zhou HJ, Hassan M, Jiang SN, Zheng JS. Ginkgolide B promotes the proliferation and differentiation of neural stem cells following cerebral ischemia/reperfusion injury, both in vivo and in vitro. Neural Regen Res. 2018;13(7):1204–1211. doi:10.4103/1673-5374.232476
160. Thid D, Benkoski JJ, Svedhem S, Kasemo B, Gold J. DHA-induced changes of supported lipid membrane morphology. Langmuir. 2007;23(11):5878–5881. doi:10.1021/la700523x
161. Yu WB, Cao L, Zhao YY, Xiao W, Xiao BG. Comparing the role of Ginkgolide B and Ginkgolide K on cultured astrocytes exposed to oxygen‑glucose deprivation. Mol Med Rep. 2018;18(5):4417–4427. doi:10.3892/mmr.2018.9450
162. Liao J, Gong L, Xu Q, et al. Revolutionizing neurocare: biomimetic nanodelivery via cell membranes. Adv Mater;2024. e2402445. doi:10.1002/adma.202402445
163. Jiang Y, Wang R, Wang C, et al. Brain microenvironment responsive and pro-angiogenic extracellular vesicle-hydrogel for promoting neurobehavioral recovery in type 2 diabetic mice after stroke. Adv Healthc Mater. 2022;11(22):e2201150. doi:10.1002/adhm.202201150
164. Bang OY, Kim EH. Mesenchymal stem cell-derived extracellular vesicle therapy for stroke: challenges and progress. Front Neurol. 2019;10:211. doi:10.3389/fneur.2019.00211
165. Reis C, Wilkinson M, Reis H, et al. A look into stem cell therapy: exploring the options for treatment of ischemic stroke. Stem Cells Int. 2017;2017:3267352. doi:10.1155/2017/3267352
166. Sakata H, Niizuma K, Yoshioka H, et al. Minocycline-preconditioned neural stem cells enhance neuroprotection after ischemic stroke in rats. J Neurosci. 2012;32(10):3462–3473. doi:10.1523/JNEUROSCI.5686-11.2012
167. Dao M, Tate CC, McGrogan M, Case CC. Comparing the angiogenic potency of naive marrow stromal cells and Notch-transfected marrow stromal cells. J Transl Med. 2013;11:81. doi:10.1186/1479-5876-11-81
168. Noiseux N, Gnecchi M, Lopez-Ilasaca M, et al. Mesenchymal stem cells overexpressing Akt dramatically repair infarcted myocardium and improve cardiac function despite infrequent cellular fusion or differentiation. Mol Ther. 2006;14(6):840–850. doi:10.1016/j.ymthe.2006.05.016
169. Lu D, Chen B, Liang Z, et al. Comparison of bone marrow mesenchymal stem cells with bone marrow-derived mononuclear cells for treatment of diabetic critical limb ischemia and foot ulcer: a double-blind, randomized, controlled trial. Diabet Res Clin Pract. 2011;92(1):26–36. doi:10.1016/j.diabres.2010.12.010
170. Abdal Dayem A, Lee SB, Kim K, et al. Production of mesenchymal stem cells through stem cell reprogramming. Int J Mol Sci. 2019;20(8):1922. doi:10.3390/ijms20081922
171. Venkat P, Chen J, Chopp M. Exosome-mediated amplification of endogenous brain repair mechanisms and brain and systemic organ interaction in modulating neurological outcome after stroke. J Cereb Blood Flow Metab. 2018;38(12):2165–2178. doi:10.1177/0271678X18782789
172. Zhang ZG, Buller B, Chopp M. Exosomes - beyond stem cells for restorative therapy in stroke and neurological injury. Nat Rev Neurol. 2019;15(4):193–203. doi:10.1038/s41582-018-0126-4
173. Kishore R, Khan M. More than tiny sacks: stem cell exosomes as cell-free modality for cardiac repair. Circ Res. 2016;118(2):330–343. doi:10.1161/CIRCRESAHA.115.307654
174. Zhang ZG, Chopp M. Neurorestorative therapies for stroke: underlying mechanisms and translation to the clinic. Lancet Neurol. 2009;8(5):491–500. doi:10.1016/S1474-4422(09)70061-4
175. Jiang X, Suenaga J, Pu H, et al. Post-stroke administration of omega-3 polyunsaturated fatty acids promotes neurovascular restoration after ischemic stroke in mice: efficacy declines with aging. Neurobiol Dis. 2019;126:62–75. doi:10.1016/j.nbd.2018.09.012
176. Fei X, Zhang X, Wang Q, et al. Xijiao dihuang decoction alleviates ischemic brain injury in MCAO rats by regulating inflammation, neurogenesis, and angiogenesis. Evid Based Complement Alternat Med. 2018;2018:5945128. doi:10.1155/2018/5945128
177. Doeppner TR, Herz J, Gorgens A, et al. Extracellular vesicles improve post-stroke neuroregeneration and prevent postischemic immunosuppression. Stem Cells Transl Med. 2015;4(10):1131–1143. doi:10.5966/sctm.2015-0078
178. Xin H, Katakowski M, Wang F, et al. MicroRNA cluster miR-17-92 cluster in exosomes enhance neuroplasticity and functional recovery after stroke in rats. Stroke. 2017;48(3):747–753. doi:10.1161/STROKEAHA.116.015204
179. Xin H, Li Y, Cui Y, Yang JJ, Zhang ZG, Chopp M. Systemic administration of exosomes released from mesenchymal stromal cells promote functional recovery and neurovascular plasticity after stroke in rats. J Cereb Blood Flow Metab. 2013;33(11):1711–1715. doi:10.1038/jcbfm.2013.152
180. Wang C, Borger V, Sardari M, et al. Mesenchymal stromal cell-derived small extracellular vesicles induce ischemic neuroprotection by modulating leukocytes and specifically neutrophils. Stroke. 2020;51(6):1825–1834. doi:10.1161/STROKEAHA.119.028012
181. De Palma M, Biziato D, Petrova TV. Microenvironmental regulation of tumour angiogenesis. Nat Rev Cancer. 2017;17(8):457–474. doi:10.1038/nrc.2017.51
182. Lee JK, Park SR, Jung BK, et al. Exosomes derived from mesenchymal stem cells suppress angiogenesis by down-regulating VEGF expression in breast cancer cells. PLoS One. 2013;8(12):e84256. doi:10.1371/journal.pone.0084256
183. Gonzalez-King H, Garcia NA, Ontoria-Oviedo I, Ciria M, Montero JA, Sepulveda P. Hypoxia Inducible Factor-1alpha Potentiates Jagged 1-mediated angiogenesis by mesenchymal stem cell-derived exosomes. Stem Cells. 2017;35(7):1747–1759. doi:10.1002/stem.2618
184. Kornhuber J, Muller CP, Becker KA, Reichel M, Gulbins E. The ceramide system as a novel antidepressant target. Trends Pharmacol Sci. 2014;35(6):293–304. doi:10.1016/j.tips.2014.04.003
185. Deng X, Yin X, Allan R, et al. Ceramide biogenesis is required for radiation-induced apoptosis in the germ line of C. elegans. Science. 2008;322(5898):110–115. doi:10.1126/science.1158111
186. Gulbins E, Palmada M, Reichel M, et al. Acid sphingomyelinase-ceramide system mediates effects of antidepressant drugs. Nat Med. 2013;19(7):934–938. doi:10.1038/nm.3214
187. Brunkhorst R, Friedlaender F, Ferreiros N, et al. Alterations of the ceramide metabolism in the peri-infarct cortex are independent of the sphingomyelinase pathway and not influenced by the acid sphingomyelinase inhibitor fluoxetine. Neural Plast. 2015;2015:503079.
188. Herr I, Martin-Villalba A, Kurz E, et al. FK506 prevents stroke-induced generation of ceramide and apoptosis signaling. Brain Res. 1999;826(2):210–219. doi:10.1016/S0006-8993(99)01288-3
189. Ohtani R, Tomimoto H, Kondo T, et al. Upregulation of ceramide and its regulating mechanism in a rat model of chronic cerebral ischemia. Brain Res. 2004;1023(1):31–40. doi:10.1016/j.brainres.2004.07.024
190. Yu ZF, Nikolova-Karakashian M, Zhou D, Cheng G, Schuchman EH, Mattson MP. Pivotal role for acidic sphingomyelinase in cerebral ischemia-induced ceramide and cytokine production, and neuronal apoptosis. J Mol Neurosci. 2000;15(2):85–97. doi:10.1385/JMN:15:2:85
191. Kanazawa M, Miura M, Toriyabe M, et al. Microglia preconditioned by oxygen-glucose deprivation promote functional recovery in ischemic rats. Sci Rep. 2017;7:42582. doi:10.1038/srep42582
192. Wattananit S, Tornero D, Graubardt N, et al. Monocyte-derived macrophages contribute to spontaneous long-term functional recovery after stroke in mice. J Neurosci. 2016;36(15):4182–4195. doi:10.1523/JNEUROSCI.4317-15.2016
193. Yu Y, Li J, Zhou H, et al. Functional importance of the TGF-beta1/Smad3 signaling pathway in oxygen-glucose-deprived (OGD) microglia and rats with cerebral ischemia. Int J Biol Macromol. 2018;116:537–544. doi:10.1016/j.ijbiomac.2018.04.113
194. Butovsky O, Jedrychowski MP, Moore CS, et al. Identification of a unique TGF-beta-dependent molecular and functional signature in microglia. Nat Neurosci. 2014;17(1):131–143. doi:10.1038/nn.3599
195. Krueger TEG, Thorek DLJ, Denmeade SR, Isaacs JT, Brennen WN. Concise Review: mesenchymal Stem Cell-Based Drug Delivery: the Good, the Bad, the Ugly, and the Promise. Stem Cells Transl Med. 2018;7(9):651–663. doi:10.1002/sctm.18-0024
196. Prockop DJ, Brenner M, Fibbe WE, et al. Defining the risks of mesenchymal stromal cell therapy. Cytotherapy. 2010;12(5):576–578. doi:10.3109/14653249.2010.507330
197. Tieu A, Slobodian M, Fergusson DA, et al. Methods and efficacy of extracellular vesicles derived from mesenchymal stromal cells in animal models of disease: a preclinical systematic review protocol. Syst Rev. 2019;8(1):322. doi:10.1186/s13643-019-1242-y
198. Go V, Bowley BGE, Pessina MA, et al. Extracellular vesicles from mesenchymal stem cells reduce microglial-mediated neuroinflammation after cortical injury in aged Rhesus monkeys. Geroscience. 2020;42(1):1–17. doi:10.1007/s11357-019-00115-w
199. Webb RL, Kaiser EE, Scoville SL, et al. Human neural stem cell extracellular vesicles improve tissue and functional recovery in the murine thromboembolic stroke model. Transl Stroke Res. 2018;9(5):530–539. doi:10.1007/s12975-017-0599-2
200. Anderson JD, Johansson HJ, Graham CS, et al. Comprehensive proteomic analysis of mesenchymal stem cell exosomes reveals modulation of angiogenesis via nuclear factor-kappaB signaling. Stem Cells. 2016;34(3):601–613. doi:10.1002/stem.2298
201. Zheng X, Zhang L, Kuang Y, et al. Extracellular vesicles derived from neural progenitor cells--a preclinical evaluation for stroke treatment in mice. Transl Stroke Res. 2021;12(1):185–203. doi:10.1007/s12975-020-00814-z
202. Yu Z, Cai Y, Deng M, et al. Fat extract promotes angiogenesis in a murine model of limb ischemia: a novel cell-free therapeutic strategy. Stem Cell Res Ther. 2018;9(1):294. doi:10.1186/s13287-018-1014-y
203. Zheng H, Yu Z, Deng M, et al. Fat extract improves fat graft survival via proangiogenic, anti-apoptotic and pro-proliferative activities. Stem Cell Res Ther. 2019;10(1):174. doi:10.1186/s13287-019-1290-1
204. Dong X, Gao J, Zhang CY, Hayworth C, Frank M, Wang Z. Neutrophil membrane-derived nanovesicles alleviate inflammation to protect mouse brain injury from ischemic stroke. ACS Nano. 2019;13(2):1272–1283. doi:10.1021/acsnano.8b06572
205. Dehaini D, Wei X, Fang RH, et al. Erythrocyte-platelet hybrid membrane coating for enhanced nanoparticle functionalization. Adv Mater. 2017;29(16). doi:10.1002/adma.201606209
206. Li M, Li J, Chen J, et al. Platelet membrane biomimetic magnetic nanocarriers for targeted delivery and in situ generation of nitric oxide in early ischemic stroke. ACS Nano. 2020;14(2):2024–2035. doi:10.1021/acsnano.9b08587
207. Xu L, Chen Y, Jin Q, et al. Biomimetic PLGA microbubbles coated with platelet membranes for early detection of myocardial ischaemia-reperfusion injury. Mol Pharm. 2021;18(8):2974–2985. doi:10.1021/acs.molpharmaceut.1c00145
208. Parvez S, Kaushik M, Ali M, et al. Dodging blood brain barrier with ”nano” warriors: novel strategy against ischemic stroke. Theranostics. 2022;12(2):689–719. doi:10.7150/thno.64806
209. Sri Kanaka Durga Vijayalakshmi G, Puvvada N. Recent advances in chemically engineered nanostructures impact on ischemic stroke treatment. ACS Omega. 2023;8(48):45188–45207. doi:10.1021/acsomega.3c06228
210. Li C, Sun T, Jiang C. Recent advances in nanomedicines for the treatment of ischemic stroke. Acta Pharm Sin B. 2021;11(7):1767–1788. doi:10.1016/j.apsb.2020.11.019
211. Wang Z, Zhao Y, Jiang Y, et al. Enhanced anti-ischemic stroke of ZL006 by T7-conjugated PEGylated liposomes drug delivery system. Sci Rep. 2015;5:12651. doi:10.1038/srep12651
212. Lv W, Xu J, Wang X, et al. Bioengineered boronic ester modified dextran polymer nanoparticles as reactive oxygen species responsive nanocarrier for ischemic stroke treatment. ACS Nano. 2018;12(6):5417–5426. doi:10.1021/acsnano.8b00477
213. Bao Q, Hu P, Xu Y, et al. Simultaneous blood-brain barrier crossing and protection for stroke treatment based on edaravone-loaded ceria nanoparticles. ACS Nano. 2018;12(7):6794–6805. doi:10.1021/acsnano.8b01994
214. Wong HL, Wu XY, Bendayan R. Nanotechnological advances for the delivery of CNS therapeutics. Adv Drug Deliv Rev. 2012;64(7):686–700. doi:10.1016/j.addr.2011.10.007
215. Saraiva C, Praca C, Ferreira R, Santos L, Ferreira L, Bernardino L. Bernardino, Nanoparticle-mediated brain drug delivery: overcoming blood-brain barrier to treat neurodegenerative diseases. J Control Release. 2016;235:34–47. doi:10.1016/j.jconrel.2016.05.044
216. Tian T, Zhang HX, He CP, et al. Surface functionalized exosomes as targeted drug delivery vehicles for cerebral ischemia therapy. Biomaterials. 2018;150:137–149. doi:10.1016/j.biomaterials.2017.10.012
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

