Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
A Systematic Review of Experimental Studies on the Impact of Empowerment-Based Interventions on Child and Parent Outcomes in the Pediatric Oncology Setting
Authors Nurhidayah I , Nurhaeni N , Allenidekania A , Gayatri D
Received 14 September 2023
Accepted for publication 21 November 2023
Published 1 December 2023 Volume 2023:16 Pages 3717—3735
DOI https://doi.org/10.2147/JMDH.S436394
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ikeu Nurhidayah,1,2 Nani Nurhaeni,3 Allenidekania Allenidekania,3 Dewi Gayatri4
1Postgraduate Program, Faculty of Nursing, Universitas Indonesia, Depok, Indonesia; 2Pediatric Nursing Department, Faculty of Nursing, Universitas Padjadjaran, Sumedang, Indonesia; 3Pediatric Nursing Department, Faculty of Nursing, Universitas Indonesia, Depok, Indonesia; 4Basic Science and Fundamental Nursing Department, Faculty of Nursing, Universitas Indonesia, Depok, Indonesia
Correspondence: Ikeu Nurhidayah, Pediatric Nursing Department, Faculty of Nursing, Universitas Padjadjaran, Sumedang, Indonesia, Email [email protected]
Background: Cancer has an impact not only on children but also on parents. Parents play the most crucial role in cancer’s symptom control and management. However, as the primary caretakers, parents are frequently unprepared or engage in inappropriate behavior when caring for their children. Increasing parents’ role through empowerment is critical in pediatric cancer care.
Purpose: This systematic review aimed to identify the effect of empowerment interventions on parent and child outcomes in pediatric oncology.
Methods: In this review, studies published between 2013 and 2023 in The Cumulative Index to Nursing and Allied Health Literature (CINAHL), PubMed, Embase, Medline, and Scopus databases were identified using a search strategy to identify relevant studies that determined empowerment-based intervention for parents in the pediatric oncology. This study used the Joanna Briggs Institute (JBI) critical appraisal tools to assess the quality of the studies. This systematic review followed the recommended reporting items for systematic reviews and meta-analysis (PRISMA) standards.
Results: Seven studies met the inclusion criteria: four randomized and three non-randomized experimental studies. Children range in age from 1– 14 years. The intervention is mostly delivered through face-to-face learning using booklets or modules as a learning tool. The intervention is delivered in 2– 6 sessions over 1– 8 weeks, lasting 20– 45 minutes each. In most studies, the interventions positively affect parents’ outcomes (knowledge, caring behavior, distress, care burden, quality of life) and children’s outcomes (oral mucositis, gastrointestinal complications, quality of life). The intervention, however, has no significant effect on the coping style. Barriers to implementation include parent-nurse commitment, the retention of parent-nurse participation, and more time spent to provide interventions.
Conclusion: Our study highlights that empowerment-based interventions positively impact parents and children. These findings suggest that an empowerment-based intervention should be developed to provide better cancer care for a parent and their children.
Systematic Review Registration: PROSPERO registration number was CRD42023422834.
Keywords: children, cancer, family, empowerment, parents
Introduction
Cancer is currently a chronic disease that endangers global health. Cancer does not only affect adults but also children. The World Health Organization (WHO) reports that the prevalence of cancer in children is around 4%.1 The majority (80%) of children with cancer are from developing countries or low and middle-income countries.2 Cancer is estimated to kill 90,000 children and adolescents each year.1 In developing countries, the survival rate for children with cancer is still relatively low, at less than 60% and even less than 30%.1,3 As a result, WHO emphasizes the importance of improving effective treatment policies for all children with cancer to increase survival rates, particularly in developing countries.1,4
Child cancer treatment is intensive and continuous, intending to control the number and spread of cancer cells and increase survival.5 The primary therapeutic modalities for treating child cancer are chemotherapy, surgery, and radiotherapy, with additional therapies including immunotherapy, photodynamic therapy, stem cell transplantation, and targeted therapy.6 Cancer treatment has numerous adverse effects on children.7 The most common side effects of cancer treatment experienced by cancer patients (69.6%) were in the mouth and gastrointestinal area.8 Other side effects of the treatment include fatigue, bone marrow depression, hair loss, and skin problems.9 In addition to the adverse side effects of the disease and its treatments, the long-term negative consequences exacerbate the negative impact on these patients’ life quality. They may cancel out any benefit of increased survival.10
Cancer has an impact not only on children but also on parents and families. Parents play the most crucial role in symptom control and management in children with cancer.11 However, as the primary caretakers for their children, parents are frequently unprepared or engage in inappropriate behavior when caring for their children. Parents face several challenges when caring for children with cancer, including a lack of knowledge, skills, and abilities.12 Parents often lack knowledge about their children’s treatment and care even though parental disease awareness is critical to child care. It is required to make appropriate decisions for children’s treatment.13 Several studies also report that parents frequently provide inadequate care for their children, necessitating appropriate and innovative interventions from health workers.14
Parents frequently perceive caring for a child with cancer as a burden.15 Parents sense a hardship since they must assume responsibility for drug administration, symptom management, and psychological well-being of sick children.16 Cancer causes life-threatening conditions and fundamental changes in the child and family.10 This condition causes parents to experience stress and anxiety, which can impact the children’s health outcomes.17
Parents must be prepared to prevent and overcome chemotherapy manifestations and the impact of cancer on children.18,19 Patient and family education, as well as holistic, supportive care strategies, are required.19,20 Parents’ abilities must be prepared so that they can provide appropriate care to their children both in the hospital and at home.19,20
Empowerment is a collaborative learning approach that is one of the fundamental concepts of family-centered care.21 Parents are the empowerment target because of their critical role in child care.12 Pediatric oncology nurses can support children and their parents through empowerment-based programs.12,22 Nurses are essential in empowering parents by providing opportunities for parents to participate in childcare activities, increasing skills and self-confidence, and preparing mothers to care for their children after they return from the hospital.23,24
Parent empowerment interventions are essential in oncology nursing. The lengthy treatment process for children’s cancer, the frequent hospitalization of children, and the long-term side effects of treatment at home necessitate continuous intervention. One of the main goals of pediatric oncology nursing is to empower parents to care for their children. Therefore, identification of the impact of empowerment-based intervention in the pediatric oncology setting is a must. Ashcraft conducted a systematic review in 2019 that identified the consequences of parent empowerment as engagement, improving informational needs, involvement in care decisions, advocacy, and empowering others.12 The studies included in Ashcraft’s review, however, were qualitative and observational, with the majority of them conducted on children with special health care needs, so generalizability to other child populations may be limited because the expected outcomes for children with special needs and children with cancer are different. Besides, because the included studies in Ashcraft’s were qualitative and observational, the review did not determine the magnitude of the effect of empowerment-based intervention on the outcomes.
In recent years, it has been seen that empowerment-based interventions are used in a wide variety, both in the format of empowerment interventions provided and their consequences. As a result, a current synthesis is required that identifies how empowerment-based interventions are carried out in pediatric oncology settings, the implications for both children and their parents, and the extent to which empowerment-based interventions influence both children and their parents. This systematic review aimed to find evidence on the impact of empowerment-based interventions on parents and their children. This systematic review will benefit the field by providing evidence for the efficacy of empowerment-based interventions for supporting and empowering children with cancer and their parents.
Materials and Methods
Study Design
This research employs a systematic review design for its study. The study protocol was registered on the PROSPERO database (CRD42023422834). The systematic review aims to inform and facilitate this process by synthesizing research from multiple studies, allowing for scale-up and efficient access to evidence.25 The framework consists of six core stages: identification of research questions, reviewing the literature, sifting the studies to select relevant ones, assessing the quality of investigations, identifying the outcome measures of each, and summarizing and reporting results.25 This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Search Method
From December 15, 2022, until March 2023, two reviewers independently analyzed research articles published between 2013 and 2023 in five databases: PubMed, The Cumulative Index to Nursing and Allied Health Literature (CINAHL), Embase, Medline, and Scopus. This study used a systematic search based on research questions aligned with medical subject headings, phrases, and combinations of synonyms with subjects on all items using Boolean (“AND” and “OR”) operators for each database. The keywords and Boolean operators used were: (“empowerment OR parent* empowerment OR family empowerment OR family center* empowerment”) AND (“child OR children”) AND (“cancer OR tumor OR malignant neoplasm”) AND (intervention OR effect).
Inclusion and Exclusion Criteria
The articles were chosen for review based on inclusion and exclusion criteria.
Inclusion Criteria
- Population: studies in which the participants are children with cancer up to 18 years old and their parents.
- Intervention: empowerment-based interventions
- Comparison: control group or standard care
- Outcome: children’s outcomes and parent’s outcomes.
- Study type: experimental studies
- The article’s publication year ranges from 2013 through 2023
Exclusion Criteria
- Studies on young adults and adult cancer patient
- Studies for children with other chronic health problems outside cancer.
- Descriptive, cross-sectional, case-control, cohort studies, qualitative studies, feasibility studies, study protocols, conference proceedings, thesis/dissertation, or abstracts.
- Studies in languages other than English
- Articles with no full text.
Study Selection and Data Extraction
Two reviewers (IN and DG) independently screened the articles from five databases. All search results were transferred into the reference management program for data management. After removing any duplicate articles, two reviewers independently reviewed and cross-checked the remaining articles. Any arguments about whether or not to include an article were settled with the help of a third reviewer (NN). Following the evaluation, the two researchers agreed. The first researcher (IN) who screened the database appraised the studies based on the appropriateness of the study title. At this stage, studies that did not match the inclusion requirements regarding the title were deleted. The reference manager application was used to record studies that satisfied the inclusion criteria in titles and abstracts, and full texts were obtained. Two independent researchers (IN and DG) evaluated full texts for inclusion criteria and methodological quality before transferring them to the data extraction table. The reviewers (IN and DG) then retrieved information from each article, including the year, study location, study design, number of samples and characteristics, the type of empowerment-based interventions employed, and theories used. The study employed the PRISMA writing criteria for systematic review and meta-analysis studies (Figure 1).
Quality Assessment
The methodological quality of the included studies was evaluated separately by two reviewers using the Joanna Briggs Institute (JBI) critical appraisal methods for experimental studies.26,27 JBI consists of 13 questions for Randomized Experimental Studies.26 Questions have four possible answers: “Yes”, “No”, “Unclear” (if no information concerning a certain issue is presented), and “Not applicable (NA)” (if a question is not done). Each question is graded either a “Yes” (1 point), a “No” (0 points), an “Unclear” (0 points), or a “Not relevant” (0 points). The overall score ranges from 0 to 13. JBI for non-randomized experimental studies consists of nine questions.27 Each question is graded as “Yes” (1 point), “No” (0 points), “Unclear” (0 points), or “Not relevant” (0 points). The overall score varied from 0 to 9 points. The high ratings achieved from both instruments imply that the study is methodologically sound. Studies that scored less than or equal to half of the items reviewed were regarded to have considerable bias, resulting in poor methodological quality. IN, DG, and AA assessed the articles critically. If there were a dispute, NN would be involved in reconciling the process based on JBI guidelines. Table 1 shows the assessments of the research using the JBI checklists developed for randomized controlled trials and non-randomized experimental studies.26,27
 |
Table 1 The JBI Critical Appraisal Tools for the Included Study |
Risk of Bias
Individual studies using experiment designs had a low risk of bias if 70% of answers were “yes”, a moderate risk if 50 to 69% of questions were “yes”, and a high risk of bias if “yes” scores were less than 50%.31 Table 2 summarizes the appraisal’s conclusion regarding the risk of bias based on the cut point, according to Viswanathan.31
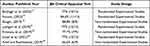 |
Table 2 The Result of Critical Appraisal for Included Studies |
Data Synthesis and Analysis
Two separate researchers build the data extraction form using the following parameters: (1) author and year, (2) country, (3) aims, (4) study design, (5) sample characteristics, (6) intervention, (7) outcomes, (8) tools, (9) measurement times, and (10) results of the study (Table 3). Table 4 summarizes the specific empowerment-based interventions carried out in each study, including data extraction: (1) author, (2) empowerment model, (3) setting, (4) empowerment steps, (5)) delivery methods, (6) media, (7) learning content, (8) frequency, (9) duration, and (10) theory/model-based.
 |
Table 3 The Primary Feature of the Systematic Review Included Studies |
 |
Table 4 The Empowerment-Based Intervention of Included Studies |
The findings are summarized, followed by a narrative describing the similarities and differences between the outcomes. The data could not be statistically assessed, and no meta-analysis could be carried out.
Results
Seven publications explored empowerment programs for cancer parents or caregivers. Table 3 and 4 highlight the findings of the analysis. Empowerment interventions for parents, especially mothers, can help them play a more significant role in caring for their children. According to Table 3, empowerment benefits the outcomes of both parents and children. The specific implementation of empowerment-based intervention can be found in Table 4. Based on the findings of this systematic review, the following is an explanation of the impact of empowerment interventions on parents of children with cancer.
Characteristics of Studies
The search yielded a total of 642 articles. After removing duplicates from the collected articles, 518 remained. Furthermore, 94 articles remained after exclusion based on the inclusion criteria. Following that, 15 articles were obtained after checking the title and abstracts. The whole text of the articles was then thoroughly assessed, and seven (7) were eventually included in this study (Figure 1). Articles were evaluated using the JBI Critical Appraisal Tool, with good article standards reaching 60% based on criteria and topic relevancy.
Table 3 shows four studies from Iran, two from Indonesia, and one from Turkey. Participants in this study were parents or caregivers of children with cancer. Three studies were conducted on mothers,13,21,29 two on parents (mothers and fathers),10,15,30 and one on the family or primary caregiver.28 The participants ranged in age from 20 to 50 years. The number of participants ranged from 40 to 78, with the lowest number found in the study by Lashgari et al21 and the highest in Shoghi’s study.15 Three studies were conducted on children with leukemia, and the remaining studies were conducted on childhood cancer in general. Children range in age from one to fourteen years.
The impact of the empowerment intervention on parental and child outcomes was assessed in the included studies. Table 3 shows that the effect of parents includes (1) knowledge of caring performance, (2) attitude and behavior, (3) distress, (4) depression, (5) coping style, (6) care burden, and (7) parental quality of life. The assessment of outcomes in children includes (1) mucositis, (2) gastrointestinal complications, and (3) children’s quality of life. Parents’ outcomes were generally measured twice in each study, before and after the intervention. The second measurement was performed at various time intervals, including one week, the 21st day after the previous session, and thirty (30) days after the last session.15
The outcomes of children, including mucositis, gastrointestinal problems, and quality of life, were assessed at various points. Mucositis was evaluated at three points: baseline, shortly following, and one month after the final intervention.10 Gastrointestinal problems were assessed at the start of the intervention, two, four, and eight weeks afterward.21 Quality of life was assessed at the beginning of the intervention and three months later.10
Characteristics of Empowerment-Based Intervention
Table 4 shows that the empowerment model implemented was the family empowerment model, mother empowerment program, parent empowerment program, and mobile-assisted empowerment. All of the studies were conducted in a hospital setting. Four studies used four steps of empowerment, including 1) threat understanding, 2) problem-solving, 3) participation, and 4) evaluation.10,13,15,21 One study used three steps,28 and two studies used two steps (providing information and family participation).29,30 The intervention period ranged from 1–8 weeks, with 2–8 sessions. The length of each intervention session ranged from 20 to 45 minutes.
Empowerment programs are mostly delivered in the form of face-to-face education training, whereas besides face-to-face training, one intervention is also equipped with groups of 3–6 parent discussions,15 while another intervention uses online learning via a mobile application.28 Booklets and pamphlets,10,13,15 educational clips and audio files,10 modules,29 and online modules,28 are among the media utilized in empowerment interventions. The educational content provided in the empowerment program includes cancer information, the signs and symptoms of cancer, diagnostic and treatment programs,15 as well as nutrition, infection prevention, and bleeding prevention,29 mucositis,10 gastrointestinal complications,21 radiotherapy side effects,28 while two other studies did not mention specific material provided.
Theories-Model Used in Intervention
According to the findings of this study, empowerment programs were developed using theories or models from the Family-centered care paradigm,13,29,30 Gibson’s Empowerment model,15 Al-Hani Iranian’s Model,10 social cognitive theory,15,21 and the quality of life paradigm.28
Parents’s Outcomes
The primary outcomes of an empowerment-based intervention for parents are knowledge of caring performance,13 caregivers or parent distress,28,29 care burden,15 coping styles,28 parents or family behavior,30 and quality of life.28
Knowledge of Caring Performance
Children rely on family care, and an active member’s role in child care is very beneficial in children’s treatment and recovery process. Parents frequently lack knowledge about the underlying cause and method of treatment and care, limiting their role in caring for their children. The Family-centered empowerment model (FCEM) intervention has improved mothers’ caregiving knowledge and prevented chemotherapy complications in children.13
Boshagh’s (2022) study found that mothers’ knowledge of caring increased after the intervention.13 Mothers, as primary caregivers for their children, can boost their self-esteem and confidence to change the situation and control the disease by sharing their experiences and information.13
Caregiver Distress and Stress Level
Cancer in children is challenging. Parents struggle to cope as they observe their children being unwell and in pain, with numerous hospitalizations and emergency visits.32,33 Parents are more likely to suffer discomfort and higher stress levels.32,33 Caregivers who participated in the empowerment program through online-based empowerment experienced less distress.28 Other studies that have been developed offer Family Centered Empowerment Module (FACE) interventions to reduce mother distress among parents.29 The FACE module has been shown to reduce stress in parents of leukemia children. Parental knowledge of dietary needs, infection control, and bleeding prevention can improve, giving parents confidence in caring for their children.29
Parents or Family Behavior in Caring for Children
Families with cancer children frequently feel powerless when attempting to balance their child’s healthcare needs with family life.17 This sense of helplessness can influence parents’ behavior when caring for children with cancer.30 Arief and Rachmawati investigated the effect of empowerment interventions on family behavior in caring for children with leukemia using a Parent Empowerment Program (PEP).30 The empowerment program is based on The Calgary Family Model. According to the study’s findings, the parent empowerment program can help families improve their knowledge, attitudes, and behavior when caring for children with cancer.
Reducing Care Burden
A study conducted by Shoghi shows that parent empowerment can reduce the care burden on parents who have children with cancer.15 The principles of the Family-Centered Empowerment Model (FCEM) are combined with an approach from The Al-Hani Empowerment Model in that study that aimed at increasing caregiver competence in caring for cancer patients receiving chemotherapy by increasing perceived threat, skill, self-efficacy, and self-confidence.15 The results of the inter-group comparison showed that the mean parental burden of care in the control group was significantly higher in the post-test than in the pre-test. In contrast, the mean parental burden of care in the intervention group decreased significantly in the post-test. Shoghi concluded that a statistically significant difference in the level of burden was observed between the two groups (p<0.001).15
Coping Style
According to Uysal’s study, cancer caregivers use coping strategies such as instrumental support, humor, emotional venting, substance use, acceptance, suppression of competing activities, religion, denial, behavioral disengagement, mental disengagement, restraint coping, and positive reframing. This study found no significant difference in coping scores between the empowerment and control groups (p ≥ 0.05).28 However, the empowerment group’s planning sub-dimensional score significantly differed in intragroup comparisons. On day 21, the empowerment group’s planning sub-dimensional score was significantly higher than the baseline score. This study concluded that caregivers in the empowerment group had higher coping scores in the planning dimension on day 21 (p=0.018).28
Improve Caregiver’s Quality of Life
The empowerment-based intervention has increased cancer caregivers’ quality of life.28 Uysal’s empowerment program is delivered through online learning via a mobile application that caregivers can access.28 The empowerment group had higher general quality of life and sub-dimensional mean scores than the control group (p≤0.05).28 According to the study, a mobile-supported empowerment program reduced caregiver distress and improved quality of life during their loved one’s radiotherapy treatment.
Children’s Outcomes
The primary outcomes of the empowerment-based intervention for children with cancer are symptom management (oral mucositis and gastrointestinal complications)10,21 and quality of life.10
Preventing Complications of Oral Mucosal Inflammation
The side effects of chemotherapy vary depending on the type and dose of drug administered to the children. Mucositis, a side effect of chemotherapy, causes inflammation and soreness in the mouth or intestine. Mucositis has been reported to affect 45–80% of children undergoing chemotherapy. According to Farsani and Moghaddasi, the Al-Hani Family Empowerment Model can help parents discover the reality and increase awareness, abilities, skills, and critical thinking in mucositis management.10 The parent empowerment program could help avoid complicating the oral mucosa’s inflammation in children undergoing chemotherapy.
Reduce Gastrointestinal Complication
According to a study by Lashgari et al, the empowerment program may improve mothers’ understanding of chemotherapy and associated difficulties, reducing such complications in chemotherapy-treated children.21 This study found that after the empowerment program in the intervention group, the frequency of gastrointestinal problems decreased significantly (p<0.05). There was no significant difference in the frequency of gastrointestinal problems before and after the intervention in the control group (p>0.05). In contrast, the intervention group had significantly fewer gastrointestinal problems than the control group after the training program.
Improve Children’s Quality of Life (QoL)
Farsani and Moghaddasi in Iran have studied the effects of empowerment programs on children’s quality of life.10 According to the study’s findings, the children’s quality of life differed significantly (p<0.001) immediately and three months after the intervention. Compared to the control group, the children in the intervention group had a significantly higher quality of life (35.12±66.30, p<0.001). There was a significant difference in the mean difference of QoL score between the intervention and control groups (4.6±7.6, p<0.001).
Discussion
In recent years, it has been stated that parent or caregiver support and empowerment interventions should be implemented throughout the cancer process.28 Empowerment as a collaborative learning approach is one of the basic concepts of family-centered care.21 In the context of child health care, parents are targets of empowerment efforts because of the integral role of parents in child care.12 Nurses not only care for children but also increase parents’ abilities through the knowledge, skills, and confidence to meet the needs of children with cancer.23
In our study, we found that an empowerment program can be delivered to mothers, parents, or carers, but we found that empowerment programs mostly targeted mothers as the primary caregivers for children. In most societies, mothers are important in children’s health care.21,34 Mothers are more often the primary caregivers for their children, while fathers have other responsibilities.35
Several studies show that strengthening mothers’ abilities is vital so that mothers can empower other family members, such as fathers, siblings, and other caregivers.15 However, fathers’ involvement in caring for children with cancer should be encouraged. A study by Shoghi in Iran found that fathers were not involved in empowerment programs because their presence in the ward was limited to visiting hours, making their accessibility difficult.15
An important finding from this systematic review is that the interventions provided varied in terms of the time and duration of the intervention. The time intervention of the empowerment-based program varies between 1–8 weeks in 2–6 sessions, with the duration varying between 20–45 minutes. The empowerment program was found to be carried out continuously over 1–8 weeks in this study rather than in a one-time shoot. According to Ashcraft et al, empowerment programs cannot be implemented in a single session because empowerment focuses on increasing knowledge and acquiring skills that direct parents to increase self-confidence or self-efficacy, obedience, and control in symptom management.12 Empowerment involves aspects of the partnership between parents and nurses. This creates a barrier to implementing the empowerment program because it requires a high level of commitment from both parties, both parents and nurses. Retention of participation by both parents and nurses is crucial to implementing an empowerment program. Therefore, Chapman and Cattaneo emphasize the need to build power and meaningful goals to increase motivation to achieve empowerment goals.36
Other findings from this study show that most empowerment-based interventions are delivered through face-to-face education, with only one study adopting web-assisted intervention as a delivery method. Discussions and question-and-answer sessions follow individual and group face-to-face education. Most studies used booklets or modules as a learning tool for parents. Only one study conducted by Uysal (2019) implemented empowerment-based technology using a mobile platform that parents can download with a smartphone.28 There are several barriers to implementing empowerment programs that use face-to-face learning; one is that they require more nurse time. This review shows that the average time nurses spent providing education was 20–45 minutes per session. A different delivery method was found in Uysal’s study, which used mobile-assisted empowerment.28 Uysal states that technological advances have provided new opportunities for planning and presenting initiatives directed toward empowerment.28 In a systematic review that examines computer-aided interventions in support of caregivers, it is stated that technology may benefit caregivers’ support.37 In Uysal’s study, the active participation of caregivers was encouraged with videos and question-answer modules.28 Apart from that, using mobile-assisted empowerment can also save nurses time spent providing education.
Another notable finding is that the entire empowerment program in this study is mainly carried out in the hospital. There were no empowerment interventions conducted in a home setting. This systematic review also found that each empowerment-based program was not followed by follow-up at home. The side effects of chemotherapy do not only occur in the hospital but can be prolonged and even worsen when the child is at home.38 As a result, empowerment programs should be long-term, provided while the child is in the hospital, and followed up on when the child returns home.39,40 Continuity of care for children with cancer is critical to ensuring that children receive appropriate care, including at home. It is hoped that parents’ ability to provide appropriate and long-term symptom care will reduce symptom suffering and severity and improve the child’s quality of life, including when the child returns home. As a result, empowerment interventions should be supplemented with a follow-up period after the child returns home from the hospital. This is required to ensure childcare continuity from hospital to home. The empowerment program’s follow-up period can be carried out not only through face-to-face meetings but also through the use of technology such as telephone, messaging, mobile applications, wearable technologies, and social media, allowing nurses to save time while maintaining nurse-parent contact even when nurses do not make home visits.41
In this study, two outcomes were observed that were influenced by the empowerment-based intervention: parent and child outcomes. This review concludes that empowerment programs significantly increase knowledge, attitudes, caring behavior, and quality of life, as well as reduce care burden and distress among parents.13,15,28–30 The relationship between empowerment-based interventions and these outcomes demonstrates that empowerment interventions can help strengthen parents’ involvement and capacities in caring for children with cancer. However, the findings of the Uysal study revealed that caregivers’ coping skills did not change even though the mobile empowerment program included information about coping with physical and psychosocial problems encountered by caregivers during the care process.28 One explanation for the finding of no changes in caregiver coping skills could be that the research time was insufficient to gain skills. Furthermore, the findings of this study revealed that empowerment programs benefit children by decreasing the frequency of chemotherapy side effects such as mucositis and gastrointestinal problems and increasing children’s quality of life.10,21
Parent empowerment is how parents gain more control over health-related decisions and actions for their children. Parents are frequently the target of empowerment efforts due to their critical role in child care.12 Parents are less confident in caring for their children.42 The study’s findings indicated that using the empowerment model to educate parents can improve parents’ caregiving knowledge and prevent chemotherapy complications in children. Well-informed parents can raise parental awareness, an essential aspect of parenting. It can increase their self-esteem and belief in their ability to change the situation and control the disease.13,43 Empowering parents is a viable alternative to improving parental knowledge and caring performance.13,44
Parents may endure substantial distress when their children are diagnosed with cancer. Uysal et al advocate for family-centered intervention that assists parents in recognizing the physical, emotional, and social needs of caregivers and the patient during cancer treatment.28 This review found that the Mobile Assisted Empowerment Program and the Family Centered Empowerment Module (FACE) programs can reduce parent distress and improve quality of life during their children’s treatment.28,29 Empowerment can reduce parental stress by giving parents the confidence to care for their children.28,29
Empowerment-based interventions may help to alleviate the burden by improving physical and mental function and increasing parents’ self-awareness.15 The majority of parents of cancer children experienced a care burden as a result of caring for their chronically ill child. Negative sensations and physical or mental effects of caring are classified as caregiver burdens.15 Living with cancer children is difficult, especially if the parents are unaware of the disease and lack professional support.45 Implementing family-based empowerment programs can help parents recognize their limitations and change their situation by providing information and support and promoting life skills.15
This study shows that empowerment-based intervention benefits reduce symptom-related chemotherapy in children. This review found that empowerment interventions benefit children by reducing the side effects of mucositis and gastrointestinal complications,10,21 thus improving the quality of life in children with cancer.10 The findings of this study show that the aspect of symptom management as a result of empowerment intervention is still limited to mucositis and gastrointestinal complications. A systematic review by Harris et al found that side effects of chemotherapy in the oral and gastrointestinal areas were the most common symptoms (69.6%) from primary studies identified, implying that these symptoms were most commonly reported by cancer patients undergoing chemotherapy.8 Therefore, the benefits of empowerment programs to reduce symptoms in the gastrointestinal system are critical in reducing the suffering of children with cancer. However, more research into developing empowerment programs to reduce chemotherapy side effects, such as pain or fatigue, should be encouraged.
Studies on empowerment-based intervention are based on theories and models such as The family-centered empowerment model (FCEM), Al-Hani Iranian’s Model, Gibson’s Empowerment Model, Social Cognitive Theory, Quality of Life Theories, and the Calgary family-centered care model.10,13,15,21,28–30 Most theoretical models used to develop the empowerment model emphasize knowledge, attitude, perceived threat, and self-efficacy. Indeed, Ashcraft’s research indicates that other aspects of empowerment, such as engagement and decision-making, require further investigation in a more comprehensive empowerment model.12
Strength and Limitations
This systematic review has some limitations. This study in this review is mostly from Asia and Eurasia, including Turkey, Iran, and Indonesia, so it is less able to provide diversity in respondents’ social and cultural characteristics. The study in this review is not focused on one type of childhood cancer or one specific outcome, which is a limitation of this review. Childhood cancers are screened in general, and no criteria for specific cancer diseases are covered in this review. The included studies revealed a wide range of consequences of empowerment. As a result, homogeneity in the outcome parameters cannot be attained, and further investigations, such as impact size calculation, cannot be done. Further study should be conducted by equalizing the type of cancer in children and focusing on specific outcomes.
Despite its limitations, this study has several benefits that should be recognized. The study used a comprehensive search strategy and systematic data extraction and quality assessment process. In addition, this review focuses on pediatric oncology settings to identify the use of empowerment-based interventions for parents and cancer children while another investigates empowerment in a broader context in the pediatric population in general or in chronic illness children population. This study included empowerment programs with various theoretical underpinnings that are appropriate for oncology settings. Thus, the findings of this study provide some strong indications of the impact of empowerment-based intervention on parent and child outcomes in oncology settings.
Implication for Nursing
The study implies a fundamental basis for health professionals, particularly pediatric nurses, to develop empowerment-based interventions for parents and children with cancer. Pediatric oncology nurses play an essential role in enhancing parents’ ability to care for their cancer children. This systematic review is expected to guide empowerment-based studies in pediatric oncology regarding the intervention used, the duration of the interventions, the key results, and the theories or models underpinning the intervention. This study also assesses the effectiveness, feasibility, and potential difficulties of using empowerment-based pediatric oncology interventions. The empowerment program in this systematic review is carried out in several sessions on an ongoing basis, which poses additional challenges, such as requiring high retention and participation from parents and nurses, implying that nurse-parents must be highly motivated to implement empowerment interventions. Another barrier is that nurses spend more time in the hospital to provide each educational session in empowerment interventions because most interventions are delivered through face-to-face learning, which reduces nurses’ time allocation for providing other direct care. Therefore, it is necessary to develop further empowerment models regarding the delivery process of the intervention to make it more effective and efficient. This research could pave the way for more comprehensive empowerment-based interventions for parents of children with cancer.
Conclusion
Our study highlights that empowerment-based interventions positively impact parents and children. There are several challenges to implementing empowerment interventions, including the need for high retention and participation from parents and nurses, as well as the need for nurses to spend more time in the hospital to provide each session of intervention. Therefore, it is necessary to develop further empowerment models regarding the delivery process of the intervention to make it more effective and efficient. These findings suggest that an empowerment-based intervention should be developed to provide better cancer care for a parent and their children.
Ethics Approval and Content to Participate
This systematic review article involved no subjects; hence, no ethical approval was required or attached.
Acknowledgment
The author would like to thank the Center for Education Financial Services of the Ministry of Education of the Republic of Indonesia in collaboration with Educational Fund Management Institution – Ministry of Finance, Republic of Indonesia, for providing doctoral scholarships to first authors through the Indonesian Education Scholarship. The authors would like to express their gratitude to Universitas Padjadjaran and Universitas Indonesia for their academic support.
Funding
Indonesian Education Scholarship for Postgraduate Program, provided by Center for Education Financial Services - The Ministry of Education, Culture, Research and Technology, Republic of Indonesia, in collaboration with Educational Fund Management Institution – Ministry of Finance, Republic of Indonesia. Recipient: Ikeu Nurhidayah, Indonesian Education Scholarship Identification Number: 202101121545.
Disclosure
The authors declare that no significant competing financial, professional, or personal interests might have affected the performance or presentation of the work described in this manuscript.
References
1. World Health Organization. WHO Global Initiative for Childhood Cancer – India Responds. Vol. 5. World Health Organization; 2020. doi:10.1016/j.phoj.2020.06.005
2. Union for International Cancer Control. Childhood Cancer ‘Signs and Symptoms’ Campaign. Union for International Cancer Control; 2017.
3. Allemani C, Weir HK, Carreira H, et al. Global surveillance of cancer survival 1995–2009: analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (Concord-2). Lancet. 2015;385(9972):977–1010. doi:10.1016/S0140-6736(14)62038-9
4. Union for International Cancer Control. Annual report leading the global fight against cancer; 2020.
5. Hockenberry M, Wilson D, Rodgers CC. Wong’s Essentials of Pediatric Nursing.
6. National Cancer Institute. Type of Cancer Treatment. Available from: https://www.cancer.gov/about-cancer/treatment/types.
7. Volberding PA, Spicer CM, Cartaxo T, Aiuppa L. Childhood Cancer and Functional Impacts Across the Care Continuum. National Academies of Sciences, Engineering, and Medicine; 2021. doi:10.17226/25944
8. Harris CS, Kober KM, Conley YP, Dhruva AA, Hammer MJ, Miaskowski CA. Symptom clusters in patients receiving chemotherapy: a systematic review. BMJ Support Palliat Care. 2022;12(1):10–21. doi:10.1136/bmjspcare-2021-003325
9. Li R, Ma J, Chan Y, Yang Q, Zhang C. Symptom clusters and influencing factors in children with acute leukemia during chemotherapy. Cancer Nurs. 2020;43(5):411–418. doi:10.1097/NCC.0000000000000716
10. Farsani NH, Moghaddasi J. The effect of family-centered empowerment model based on mucosal management on the quality of life of children with cancer undergoing chemotherapy. Res Sq. 2023;7(2):1–20.
11. Friedrichsdorf SJ, Postier A, Dreyfus J, Osenga K, Sencer S, Wolfe J. Improved quality of life at end of life related to home-based palliative care in children with cancer. J Palliat Med. 2015;18(2):143–150. doi:10.1089/jpm.2014.0285
12. Ashcraft LE, Asato M, Houtrow AJ, Kavalieratos D, Miller E, Ray KN. Parent empowerment in pediatric health care settings: a systematic review of observational studies synthesis of results: we identified six themes within consequences of empowerment: increased parent involvement in daily care, improved symptom management. Patient. 2019;12(2):199–212. doi:10.1007/s40271-018-0336-2.Parent
13. Boshagh F, Hakim A, Alghasi A, Haghighizadeh MH. Effect of family-centered empowerment model on knowledge and caring performance of mothers of children with leukemia: a randomized clinical trial. Jundishapur J Chronic Dis Care. 2022;11(3):1–7. doi:10.5812/jjcdc-116854.Research
14. Uhl K, Burns M, Hale A, Coakley R. The critical role of parents in pediatric cancer-related pain management: a review and call to action. Curr Oncol Rep. 2020;22(4). doi:10.1007/s11912-020-0899-7
15. Shoghi M, Shahbazi B, Seyedfatemi N. The effect of the Family-Centered Empowerment Model (FCEM) on the care burden of the parents of children diagnosed with cancer. Asian Pacific J Cancer Prev. 2019;20(6):1757–1764. doi:10.31557/APJCP.2019.20.6.1757
16. Flury M, Caflisch U, Ullmann-Bremi A, Spichiger E. Experiences of parents with caring for their child after a cancer diagnosis. J Pediatr Oncol Nurs. 2011;28(3):143–153. doi:10.1177/1043454210378015
17. Lewandowska A. Influence of a child’s cancer on the functioning of their family. Children. 2021;8(7):592. doi:10.3390/children8070592
18. Cheng KKF. Oral mucositis: a phenomenological study of pediatric patients’ and their parents’ perspectives and experiences. Support Care Cancer. 2009;17(7):829–837. doi:10.1007/s00520-009-0618-2
19. Alkhuwaiter S. Parents’ awareness and oral health care measures of pediatric patients receiving chemotherapy. J Pediatr Dent. 2021;7(1). doi:10.14744/jpd.2021.04_38
20. Cheng KKF, Tan LML. A pilot study of the effect of a home-based multimodal symptom-management program in children and adolescents undergoing chemotherapy. Cancer Rep. 2021;4(3):e1336. doi:10.1002/cnr2.1336
21. Lashgari L, Manesh SJ, Naeni MK. Effect of maternal empowerment training on frequency of gastrointestinal complications in children undergoing chemotherapy. J Res Dev Nurs Midw. 2021;18(2):41–48. doi:10.29252/jgbfnm.18.2.41
22. Damen H, Scholte RHJ, Vermulst AA, van Steensel P, Veerman JW. Parental empowerment as a buffer between parental stress and child behavioral problems after family treatment. Child Youth Serv Rev. 2021;124(March):105982. doi:10.1016/j.childyouth.2021.105982
23. Panicker L. Nurses’ perceptions of parent empowerment in chronic illness. Contemp Nurse. 2013;45(2):210–219. doi:10.5172/conu.2013.45.2.210
24. Borhani F, Najafi MK, Rabori ED, Sabzevari S. The effect of family-centered empowerment model on quality of life of school-aged children with thalassemia major. Iran J Nurs Midwifery Res. 2011;16(4):292–298.
25. Gopalakrishnan S, Ganeshkumar P. Systematic reviews and meta-analysis: understanding the best evidence in primary healthcare. J Fam Med Prim Care. 2013;2(1):9. doi:10.4103/2249-4863.109934
26. Barker TH, Stone JC, Sears K, et al. The revised JBI critical appraisal tool for the assessment of risk of bias for randomized controlled trials. JBI Evid Synth. 2023;21(3):494–506. doi:10.11124/JBIES-22-00430
27. Tufanaru C, Munn Z, Aromataris E, Campbell J, Hopp L. Systematic reviews of effectiveness. In: JBI Manual for Evidence Synthesis. Joanna Briggs Institute; 2020. https://synthesismanual.jbi.global/.
28. Uysal N, Bağçivan G, Özkaraman A, et al. Empowering caregivers in the radiotherapy process: the results of a randomized controlled trial. Support Care Cancer. 2021;29(5):2395–2404. doi:10.1007/s00520-020-05743-z
29. Krisnana I, Sulistyarini H, Rachmawati PD, Arief YS, Kurnia ID. Reducing acute stress disorders in mothers of leukemic children by means of the family Centered Empowerment Module (FACE). Cent Eur J Nurs Midwifery. 2019;10(2):1035–1040. doi:10.15452/CEJNM.2019.10.0011
30. Arief YS, Rachmawati PD. Parent empowerment program in caring for children with leukemia. Enferm Clin. 2019;29:897–899. doi:10.1016/j.enfcli.2019.04.136
31. Viswanathan M, Ansari MT, Berkman NDN, et al. Assessing the risk of bias of individual studies in systematic reviews of health care interventions - methods guide – chapter | AHRQ effective health care program. Methods Guid Eff Comp Eff Rev. 2012. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22479713. Accessed November 21, 2023.
32. Phipps S, Long A, Hudson M, Rai SN. Symptoms of post-traumatic stress in children with cancer and their parents: effects of informant and time from diagnosis. Pediatr Blood Cancer. 2005;45(7):952–959. doi:10.1002/pbc.20373
33. Masa’deh R, Jarrah S. Post traumatic stress disorder in parents of children with cancer in Jordan. Arch Psychiatr Nurs. 2017;31(1):8–12. doi:10.1016/j.apnu.2016.07.012
34. Vieira AC, da Rocha Cunha ML. My role and responsibility: mothers’ perspectives on overload in caring for children with cancer. Rev da Esc Enferm. 2020;54:1–9. doi:10.1590/S1980-220X2018034603540
35. Vieira AC, da Rocha Cunha ML, Neris RR, et al. Caring for a child with cancer: impact on mother’s health. Rev da Esc Enferm. 2020;55(3):1731–1738. doi:10.7314/APJCP.2014.15.4.1731
36. Cattaneo LB, Chapman AR. The process of empowerment: a model for use in research and practice. Am Psychol. 2010;65(7):646–659. doi:10.1037/a0018854
37. McKechnie V, Barker C, Stott J. Effectiveness of computer-mediated interventions for informal carers of people with dementia - a systematic review. Int Psychogeriatr. 2014;26(10):1619–1637. doi:10.1017/S1041610214001045
38. Duran J, Bravo L, Torres V, et al. Quality of life and pain experienced by children and adolescents with cancer at home following discharge from the hospital. J Pediatr Hematol Oncol. 2020;42(1):46–52. doi:10.1097/MPH.0000000000001605
39. Torres-Espíndola LM, Demetrio-Ríos J, Carmona-Aparicio L, et al. Comorbidity index as a predictor of mortality in pediatric patients with solid tumors. Front Pediatr. 2019;7(MAR):1–7. doi:10.3389/fped.2019.00048
40. Torres V, Nunes MDR, Silva-Rodrigues FM, et al. Frequency, severity, and distress associated with physical and psychosocial symptoms at home in children and adolescents with cancer. J Pediatr Healthc. 2019;33(4):404–414. doi:10.1016/j.pedhc.2018.11.007
41. Ozdemir Koyu H, Kilicarslan Törüner E. The effect of technology-based interventions on child and parent outcomes in pediatric oncology: a systemic review of experimental evidence. Asia Pac J Oncol Nurs. 2023;10(5). doi:10.1016/j.apjon.2023.100219
42. Bedells E, Bevan A. Roles of nurses and parents caring for hospitalised children. Nurs Child Young People. 2016;28(2):24–28. doi:10.7748/ncyp.28.2.24.s22
43. Rajabi R, Forozy M, Fuladvandi M, Eslami H, Asadabady A. The effect of family-centered empowerment model on the knowledge, attitudes and self-efficacy of mothers of children with asthma. J Nurs Educ. 2016;5(4):41–50. doi:10.21859/jne-05046
44. Sisk BA, Mack JW, Ashworth R, DuBois J. Communication in pediatric oncology: state of the field and research agenda. Pediatr Blood Cancer. 2018;65(1):1–10. doi:10.1002/pbc.26727
45. Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS. Caregiver burden: a clinical review. JAMA. 2014;311(10):1052–1059. doi:10.1001/jama.2014.304
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

