Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 12
Condom Utilization and Affecting Factors Among People Living with HIV/AIDS Attending ART Clinics in Addis Ababa, Ethiopia
Authors Geleta RH, Tiruneh MA
Received 15 August 2020
Accepted for publication 25 September 2020
Published 19 October 2020 Volume 2020:12 Pages 583—590
DOI https://doi.org/10.2147/HIV.S276802
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Bassel Sawaya
Rahel Hailu Geleta,1 Mesafint Abeje Tiruneh2
1Nefas Silk Lafto Sub City Woreda 5 Health Center, Addis Ababa, Ethiopia; 2Bethzatha General Hospital, Addis Ababa, Ethiopia
Correspondence: Rahel Hailu Geleta Nefas Silk Lafto Sub City Woreda 5 Health Center, Addis Ababa, Ethiopia
Tel +251913551027
Email [email protected]
Background: Human immune deficiency virus or acquired immune deficiency syndrome (HIV/AIDS) has been a major public health problem globally as well as in Africa including Ethiopia. To prevent HIV effectively, condoms must be used regularly and consistently. When HIV positive individuals have sex without condom, they can easily transmit the vuirus to a seronegative partner. Condom utilization may be affected by various factors. Therefore, the findings from this study will give an opportunity to understand condom utilization and the barriers to condom use.
Objective: To assess condom utilization and associated factors among people living with HIV/AIDS attending anti-retro viral treatment (ART) clinics in Addis Ababa, Ethiopia.
Materials and Methods: An institution-based cross-sectional study was conducted among 677 people living with HIV/AIDS attending ART clinics in Addis Ababa from February 1, 2019 to March 30, 2019. The sampling technique was three-stage sampling and finally, the study participants were selected using a systematic random sampling technique. Data were coded, cleaned and entered in to EPIData version 3.4, and analyzed using SPSS version 23.0. The association between the dependent variable and independent variables was analyzed using binary logistic regression analysis at 5% level of significance.
Results: About 677 HIV/AIDS patients receiving ART at health centers participated in the study. From the total participants, 306 (45.2%) utilized a condom in the last six months. Sex (adjusted odds ratio (AOR)=2.02; 95%CI=1.34– 3.05), marital status (AOR=0.39; 95%CI=0.19– 0.77 and (AOR=0.48; 95%CI=0.24– 0.94), employment status (AOR=0.27; 95%CI=0.12– 0.59), type of partner (AOR=0.15; 95%CI=0.05– 0.48 and AOR=0.46; 95%CI=0.27– 0.79), condom access (AOR=3.97; 95%CI=2.04– 7.75), disclosure of HIV status (AOR=0.21; 95%CI=0.14– 0.33) and attitude towards condoms (AOR=3.76; 95%CI=2.49– 5.65) had significant association with condom utilization.
Conclusion: Condom utilization was found to be low among people living with HIV/AIDS attending ART clinics in Addis Ababa. This finding indicates that high concern shall be given to minimize the gap. Sex, marital status, employment status, disclosure of HIV status, condom access, type of partner and attitude towards condoms were significantly associated with condom utilization. Hence, continuous condom provision, promotion, demonstration, and awareness creation are vital.
Keywords: condom utilization, HIV/AIDS, anti-retroviral therapy, Addis Ababa, Ethiopia
Introduction
Globally, HIV epidemic threats to public health were recognized 30 years ago.1 Seventy-six point one million people became infected with HIV and 35.0 million people died due to HIV/AIDS since the start of the epidemic.2 Thirty-six point seven million people were living with HIV, 1.8 million people became newly infected with HIV and one million people died from AIDS 2016 globally.2 Young women aged 15–24 years are at particularly high risk of HIV infection among adults globally in 2015.3 Globally about 45 million HIV infections have been prevented through condom use since 1990 globally.4 In 2015, an estimated 1.9 million adults were newly infected with HIV, most of them were infected through sexual intercourse.5
Nineteen point four million people were living with HIV in Eastern and Southern Africa in 2016.2 In Sub-Saharan Africa, HIV/AIDS has been a major health problem for more than 20 years. Even if Ethiopia has one of the lowest HIV prevalence rates in East Africa, still there are more than one million people living with HIV.6 Over the last decade free anti-retro viral treatment (ART) services scale-up in the country has been one of the achievements of the HIV/AIDS program. The scale-up of ART program services have substantially decreased deaths and contributed to reduce incidence of HIV since the initiation of the ART program in 2005.7
Even though there is progress, the benefits of condom utilizations are not fully being used.1 Condoms must be used consistently and correctly to achieve the high level of protection against HIV.8 Epidemiologic and laboratory studies indicates a condom is effective for HIV and sexually transmitted diseases (STD) prevention.9 Inconsistent or incorrect use of condoms usually leads to failure to protect against STD/HIV transmission.8 Transmission of HIV and STDs can occur with a single sex act with an infected partner due to inconsistent or nonuse of condoms. Incorrect use of condoms minimizes the effectiveness of condoms by leading to leakage, breakage, or slippage.9
Many people living with HIV have partners who have not acquired HIV, sero-discordant couples. Couple and partner testing, consistent condom use and providing ART to the partner living with HIV are key prevention strategies for sero-discordant couples.1 Condom use is important even if both partners have HIV to prevent re-infection.10 Key populations including sex workers, people who inject drugs, transgender people, prisoners, and gay men and other men who have sex with men have higher risk of HIV infection.11
Knowledge of HIV prevention methods is low in Ethiopia. Only 56% of women knew that HIV could be prevented using condoms and only 65% knew that HIV could be prevented by limiting sex to one uninfected partner in 2011. Multiple sexual partners without using a condom increases the risk of contracting HIV.6 If HIV-positive individuals have sex without a condom, individuals with low CD4 count or higher viral load at the initiation of ART have the potential to transmit to a sero-negative sexual partner or they may be at risk of acquiring drug-resistant viral strains.12
Since unprotected sexual intercourse with an HIV-infected person easily transmits infection, inconsistent and incorrect use of condoms will increase the disease incidence and prevalence. In Ethiopia condom promotion and distribution is emphasized for the general population rather for PLWHA, therefore, data regarding condom use are hardly found. Despite the fact that condoms are the most effective method to fight against HIV/AIDS there is little information regarding its magnitude and the factors affecting condom utilization among PLWHA.13
Data regarding condom utilization among PLWHA are rare to find in Ethiopia. Therefore, this study tries to assess condom utilization among PLWHA receiving ART and the factors that affect their utilization in Addis Ababa such as sociodemographic factors, knowledge and attitude related factors, condom access, type of partner, disclosure of HIV status, duration on ART and substance use. The government offices and nongovernmental organizations (NGOs) working in this area will gain insight from the findings that may help them identify the gaps and plan appropriate intervention methods to improve condom utilization while increasing its provision and making it acceptable among PLWHA.
Materials and Methods
Study Design and Setting
Institution-based cross-sectional study was conducted in Addis Ababa, Ethiopia from February, 1, 2019 to March 30, 2019. According to the last national census in 2007, the city has an estimated total population of 3,384,569. There are 10 sub-cities in Addis Ababa. The city accompanied 93 health centers within the 10 sub-cities which is divided by woredas and majority of them provide ART service. It has the second highest HIV/AIDS prevalence rate in the country 3(.4%), according to the 2018 Federal HIV/AIDS Prevention and Control Office report.14
Source and Study Population
The source population were PLWHA attending ART clinics of health centers in Addis Ababa and the study population were PLWHA attending ART clinics of selected health centers in Addis Ababa. PLWHA aged above 18 years who had been on ART for at least one month prior to the data collection period were included in the study. Critically ill and those who were unable to respond were excluded from the study.
Sample Size Determination and Sampling Procedure
Double population proportion formula was used to determine the sample size by considering 95%CI, 80% power and one-to-one ratio based on a study conducted in North West Ethiopia, 201513 by Epi info statistical calculation. Design effect, 1.5 and 10% nonresponse rate were considered and the final sample size was 677.
Three-stage sampling technique was used. There are 10 sub-cities in the city from these three sub-cities were selected using a simple random sampling technique. The selected three sub-cities had 17 health centers which provide ART service. Six health centers were selected from the two sub-cities (three from each) and two health centers were selected from the third sub-city using simple random sampling technique proportion to the number of health centers; a total of eight health centers were selected. A systematic random sampling technique was used to select the study participants who were interviewed after the first random start proportional to the number of patients in each health center.
Operational Definitions
Condom utilization: whether the study participants used condoms regularly and consistently in the last six months prior to the study.
Knowledge about condom use:
Knowledgeable: study participants who answered at least five of the seven knowledge-related questions about condoms.
Not knowledgeable: study participants who answered less than five of the seven knowledge-related questions about condoms.
Attitude toward condom use:
Favorable attitude: study participants who answered two of the three attitude-related questions toward condom use.
Unfavorable attitude: study participants who answered less than two of the three attitude-related questions toward condom use.
Knowledge about HIV/AIDS:
Knowledgeable: study participants who answered three of the five knowledge-related questions about HIV/AIDS transmission and prevention practice.
Not knowledgeable: study participants who answered less than three of the five knowledge-related questions about HIV/AIDS transmission and prevention practice.
Attitude towards HIV/AIDS:
Favorable attitude: study participants who answered at least one of the two attitude-related questions towards HIV/AIDS transmission and prevention practice.
Unfavorable attitude: study participants who answered none of the two attitude-related questions towards HIV/AIDS transmission and prevention practice.
Data Collection Tool, Procedure and Quality Assurance
A structured interviewer administered questionnaire was first prepared in English and then translated in to Amharic. The data was collected using the Amharic version questionnaire. The questionnaire was then back translated into English for data entry. In order to assure the quality of the data, training was given to three selected health care professional data collectors who were not working in those health centers where the study was conducted and pretest was done on 5% of the study participants who were not included in the actual study. The collected data were checked for completeness and consistency daily during the data collection period.
Data Management and Data Analysis
The data collected from each participant was coded and entered in to EpiData version 3.4 and then exported to SPSS version 23 computer software for analysis. Relevant descriptive statistics such as frequency and percent were carried out. To screen out potentially significant variables, univariate binary logistic regression analysis was done, and those with less than 25% level of significance remained in the final models. To check the adequacy of the final model Hosmer–Lemeshow goodness of fit test was used (p=0.08). Multicollinearity test was done and no multicollinearity identified. Sensitivity analysis done and no data bias detected. Finally, a stepwise multiple binary logistic regression analysis was done. Adjusted odds ratio and 95%CI was employed to examine associations. Variables with p-value <0.05 were considered as statistically significant.
Results
Sociodemographic Characteristics of the Study Population
The total study participants were 677 in number, with an age range of 20–65 years and the mean age was 38.5 (SD±5.5) years. There were more females constituting 415 (61.3%) of the total study participants. The majority of the participants 453 (66.9%) were orthodox Christians. From the total participants 232 (34.3%) were married. More than one-third of the study participants 321 (47.4%) were self-employed while one-third of the participants 226 (33.4%) had completed secondary education and 116 (17.1%) had no formal education (Table 1).
 |
Table 1 Sociodemographic Characteristics of Study Participants, Addis Ababa, 2019 (n=677) |
Knowledge and Attitude About HIV/AIDS, Condoms and their Utilization
The majority, 469 (69.3%) of the study participants were knowledgeable about HIV/AIDS transmission and prevention practice. About 534 (78.9%) of the total participants had a favorable attitude toward HIV/AID prevention practice. About 479 (70.8%) of the total respondents were knowledgeable about condoms and 358 (52.9%) respondents had a favorable attitude toward condom use (Table 2).
 |
Table 2 Knowledge and Attitude About HIV/AIDS, Condoms and Their Utilization Among Study Participants, Addis Ababa, 2019 (n=677) |
Condom Access and Type of Partner
About 517 (76.4%) of the total respondents had a regular sexual partner/spouse in the last six months while the rest 24 (3.5%) and 136 (20.1%) of the respondents engaged in sexual relationships with sex workers and multiple partners, respectively (Table 3).
 |
Table 3 Condom Access and the Type of Partner Among Participants, Addis Ababa, 2019 (n=677) |
Approximately 593 (87.6%) of the respondents had access to condoms and the rest 84 (12.4%) had not from the respondents who had no access to condoms the reasons stated were price 5 (6%), distance/nonavailability 20 (23.8%), preference/type of condom 1 (1.2%), fear of being seen when buying 20 (23.8%) and did not know where to find 38 (45.2%) (Figure 1).
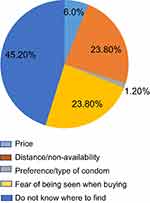 |
Figure 1 Reason for nonaccessibility of condom among respondents, Addis Ababa, 2019 (n=677). |
Duration on ART, Substance Abuse and Disclosure About HIV Status
About 22 (3.2%) of the total respondents stayed on ART for <3 months while nearly half of them 356 (52.6%) stayed on ART for more than 36 months.
About 131 (19.4%) of the respondents had used at least one of the substances (alcohol, cigarette, or chat) while engaging in a sexual relationship. Regarding disclosure about HIV status, more than half 392 (57.9%) of the respondents did not inform their partners of their HIV status (Table 4).
 |
Table 4 Duration on ART, Substance Abuse, Disclosure About HIV Status Among Participants, Addis Ababa, 2019 (n=677) |
Condom Utilization
Among the total study participants, 306 (45.2%, 95%CI=41.5–49.0%) reported that they used condoms regularly and consistently whereas the remaining 371 (54.8%, 95%CI: 51.0–58.5%) respondents did not used condoms regularly and consistently in the last six months.
Factors Associated with Condom Utilization
At a 25% level of significance univariate binary logistic regression analysis of sex, educational status, marital status, employment status, condom access, knowledge about HIV, attitude toward condoms, type of partner and disclosure of HIV status were significantly associated with condom utilization. However, at a 5% level of significance multivariable binary logistic regression analysis of sex, marital status, employment status, type of partner, condom access, disclosure of HIV status and attitude toward condoms were significantly associated with condom utilization.
Male respondents were 2.02 times more likely to utilize condom compared to female respondents (AOR=2.02; 95%CI=1.34–3.05). Respondents who were married and widowed were 61% and 52% less likely to utilize condom, respectively when compared to those who were single (AOR=0.39; 95%CI=0.19–0.77 and (AOR=0.48; 95%CI=0.24–0.94)
Similarly, respondents who were self-employed/business were 73% less likely to utilize condom compared to unemployed respondents (AOR=0.27; 95%CI=0.12–0.59). Respondents who had multiple sexual partners and who had sex with sex workers were 85% and 54% less likely to utilize condoms compared to those who had regular sexual partner, respectively (AOR=0.15; 95%CI=0.05–0.48 and AOR=0.46; 95%CI=0.27–0.79).
Respondents who had access to condoms were 3.97 times more likely to utilize them compared to respondents who had no access (AOR=3.97; 95%CI=2.04–7.75). Respondents who did not disclose their HIV status to their partners were 79% less likely to utilize condoms compared to respondents who disclosed their status (AOR=0.21; 95%CI=0.14–0.33).
Respondents who had a favorable attitude toward condoms were 3.76 times more likely to utilize condoms than those who had an unfavorable attitude (AOR=3.76; 95%CI=2.49–5.65) (Table 5).
 |
Table 5 Factors Associated with Condom Utilization Among PLWHA Attending ART Clinics in Addis Ababa, 2019 (n=677) |
Discussion
The finding of this study showed that the proportion of condom utilization is 45.2%, this finding is similar to the study of condom utilization among people living with HIV/AIDS attending ART clinic in North Central Nigeria (45.5%).15 However, this finding is quite different from the study on consistent condom use in HIV/AIDS patients receiving ART in northwest Ethiopia (78.9%).13
This study showed that consistent condom use is affected by sex. Male respondents were 2.02 times more likely to utilize condom than female respondents. This finding is similar to the studies conducted in North Central Nigeria, in Northwest Ethiopia and in the Asia-Pacific Region.15,16 This might be due to the fact that women are less powerful to negotiate condom use and have less ability to decide on sexual life especially in developing countries. Women also involve in risky sexual behaviors due to economic problems and they might be forced not to use condoms either due to extra payment or inability to negotiate.
This study also showed that there is a significant association between disclosure of HIV status and condom utilization. Respondents who did not disclose their HIV status to their partners were 79% less likely to utilize condoms than respondents who disclosed their status. This finding is consistent with the study conducted among PLWHA in Maiduguri, Nigeria.17 This shows that individuals do not bother about knowing their partners HIV status and they may have fear that if their partners are sero-negative, they might leave them and e remain alone or not to be blamed by their partners if they become positive after the relationship.
Respondents who were married and widowed were 61% and 52% less likely to utilize condoms, respectively when compared to those who were single and this finding is in agreement with a study conducted in Maiduguri, Nigeria.17 This may be due to the perception that a condom is unnecessary among married couples, partners refusal of condom, the desire to have children and less empowerment for women.
There is also an association between occupational status and condom utilization. Respondents who were self-employed/business were 73% less likely to utilize condoms compared to unemployed respondents. Respondents who had multiple sexual partners and who had sex with sex workers were 85% and 54% less likely to utilize condoms compared to those who had a regular sexual partner, respectively. This indicates that despite the efforts made through counseling to decrease HIV transmission and re-infection people are still involved in risky sexual behaviors which could result in further spread of HIV infection in the society and treatment failure in PLWHA.
Respondents who had access to condoms were 3.97 times more likely to utilize them compared to respondents who had no access. This finding is supported by a systematic review done in the Asia-Pacific region.16 This might be due to individuals do not knowing where to find condoms, being ashamed to buy condoms openly or nonavailability (the condoms from clinics may not sustain them till the next visit).
Respondents who had a favorable attitude toward condoms were 3.76 times more likely to utilize condoms than those who had an unfavorable attitude. This may be due to the misperception that condoms decrease sexual pleasure and being in ART totally prevents HIV.
Limitation of the Study
Although this study provides important information regarding condom utilization and its determinant factors, which is relevant to make interventions, it may have certain limitations of recall and socially desirable bias.
Conclusion
Condom utilization was found to be low among people living with HIV/AIDS attending ART clinics in Addis Ababa. This finding indicates that high concern shall be given to minimize the gap. Sex, marital status, employment status, discloses of HIV status, condom access, type of partner and attitude toward condoms were significantly associated with condom utilization. Therefore, continuous condom provision, promotion, demonstration and awareness creation are vital. Community based education and sensitization on HIV/AIDS and condom use has to be a major concern of stakeholders. Health-care providers should create awareness among PLWHA that condom use is the key intervention to prevent HIV transmission and reinfection including its negative outcome and the need to use condoms even with in marriage.
Data Sharing Statement
All relevant data are available within the manuscript.
Ethics Approval and Consent to Participate
As our institutions do not have the mandate to provide ethical clearance for research, ethical clearance was obtained from GAMBY Medical and Business College and Addis Ababa Health Bureau. This study was conducted under technical support and supervision of GAMBY Medical and Business College. The findings of the study were also presented to the College and approved. The study was conducted in accordance with the Declaration of Helsinki. The study participants were informed that participation was voluntarily and written informed consent was taken from the study participants by telling that they have the right not to respond. This study had no risk for study participants. Confidentiality of the collected data was maintained using a code number instead of their name.
Consent for Publication
Consent for publication was taken from the study participant during data collection.
Acknowledgments
Authors would like to thank all study participants, data collectors and GAMBY Medical and Business College and Addis Ababa Health Bureau.
Author Contributions
Both authors meet the ICMJE criteria for co-authorship, providing substantial intellectual contributions for the manuscript. Both authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors received no specific funding for this research.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. Global Update on the Health Sector Response to HIV. 2014.
2. United Nations Program for HIV/AIDS. Global HIV Statistics Fact Sheet-World AIDS Day. 2017.
3. United Nations Program for HIV/AIDS. Global AIDS Update. 2016.
4. Stover J, Avenir H. The Contribution of Condoms to HIV Prevention. Presentation Made at Global Condom Steering Group Meeting. 2016.
5. Lori N, Jane R, Stephen V, et al. Global estimates of the prevalence and incidence of four curable sexually transmitted infections in 2012 based on systematic review and global reporting. PLoS One. 2015;10(12):1–17.
6. Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2011. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF; 2011.
7. Federal Democratic Republic of Ethiopia. Country Progress Report on the HIV Response. 2014.
8. United States Aid for International Development. Condom Fact Sheet. 2015.
9. Center for Communicable Disease ontrol. Condom Fact Sheet in Brief.department of Health and Human Service. 2013.
10. UNFPA, WHO, PATH. Condom Programing for HIV Prevention an Operational Manual for Programme Managers. 2005.
11. United Nations Program for HIV/AIDS. Prevention Gap Report. 2016.
12. Donnell D, Baeten J, Kiarie J. Partners in prevention HSV/HIV transmission study team. Heterosexual HIV-1 transmission after initiation of antiretroviral therapy: a prospective cohort analysis. Lancet. 2010;375(9731):2092–2098. doi:10.1016/S0140-6736(10)60705-2
13. Zewdneh S, Befikadu L, Bayew T, Akshaya S, Abyot E. Consistent condom use in HIV/AIDS patients receiving antiretroviral therapy in Northwestern Ethiopia: implication to reduce transmission and multiple infections. HIV AIDS. 2015;7:119–124.
14. Ethiopian Federal HIV/AIDS Prevention and Control Office. Annual Report. 2018.
15. Adekunle G, Salaudeen OI, Yusuf A, et al. Condom use among people living with HIV/AIDS attending Abejukolo General Hospital in Kogi State, North Central Nigeria. Ann Afr Med. 2014;13(3):99–103. doi:10.4103/1596-3519.134378
16. Keshab D, Verena K, Sushil K, Anna M. Condom use behaviour among people living with HIV: a seven-country community-based participatory research in the Asia-Pacific region. BMJ. 2017;1–8.
17. Ballah A, Sasilu A, David B, Umaru I, Babajide B. Evaluation of condom use and associated factors adult HIV clients in Maiduguri, North Eastern Nigeria: a comparative cross sectional study. World J AIDS. 2014;4(02):169–177. doi:10.4236/wja.2014.42022
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
