Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 16
Detection of Thyroid Nodule Prevalence and Associated Risk Factors in Southwest China: A Study of 45,023 Individuals Undergoing Physical Examinations
Authors Liang Y, Li X, Wang F, Yan Z, Sang Y, Yuan Y, Qin Y, Zhang X, Ju M
Received 31 March 2023
Accepted for publication 3 June 2023
Published 8 June 2023 Volume 2023:16 Pages 1697—1707
DOI https://doi.org/10.2147/DMSO.S412567
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Juei-Tang Cheng
Yi Liang,1,2 Xiaohong Li,1 Fang Wang,2 Zongting Yan,2 Yuhuan Sang,2 Yuan Yuan,2 Yun Qin,1 Xuefei Zhang,1 Mei Ju2
1Health Management Center, Affiliated Hospital of Southwest Medical University, Luzhou, Sichuan, 646000, People’s Republic of China; 2Nursing College, Southwest Medical University, Luzhou, Sichuan, 646000, People’s Republic of China
Correspondence: Mei Ju; Xiaohong Li, Email [email protected]; [email protected]
Background: Thyroid nodules (TNs) are among the most common thyroid lesions, and rates of these nodules have risen over the past three decades. As the majority of TN patients remain asymptomatic when these nodules are in the early stages of development, malignant nodules may continue to develop into thyroid cancer when not detected. As such, early screening and diagnosis-based strategies represent the most promising means of preventing or treating TNs and associated cancers. The present study was thus developed to explore TN prevalence among individuals in Luzhou, China.
Methods: Here, thyroid ultrasonography and metabolic-related indicators from 45,023 adults undergoing routine physical examinations in the Health Management Center of a large Grade A hospital in Luzhou over the last three years were retrospectively reviewed in an effort to identify factors associated with TN risk and the detection of these nodules through univariate and multivariate logistic regression analyses.
Results: In total, 13,437 TNs were detected in these 45,023 healthy adults for an overall 29.8% detection rate. This TN detection rate rose with age, and multivariate logistic regression analyses revealed that independent risk factors associated with TNs included greater age (≥ 31 years old), female (OR = 2.283, 95% CI: 2.177– 2.393), central obesity (OR = 1.115, 95% CI: 1.051– 1.183), impaired fasting glucose (OR = 1.203, 95% CI: 1.063– 1.360), overweight status (OR = 1.085, 95% CI: 1.026– 1.147), and obesity (OR = 1.156, 95% CI: 1.054– 1.268), while low BMI was a protective factor associated with lower rates of TN incidence (OR = 0.789, 95% CI: 0.706– 0.882). When results were stratified by gender, impaired fasting glucose was not an independent predictor of TN risk among males, while high LDL levels were an independent predictor of TNs among females, and other risk factors were not significantly changed.
Conclusion: TN detection rates were high among adults in Southwestern China. Female, elderly individuals, individuals exhibiting central obesity, and those with high levels of fasting plasma glucose are more likely to develop TN.
Keywords: thyroid nodules, detection rate, influence factors
Introduction
The thyroid gland, consisting of two connected lobes, is one of the largest endocrine glands in the human body, weighing 20–30 g in adults. Thyroid lesions are often found on the gland, with a prevalence of 4–7%. Most of them are asymptomatic, and thyroid hormone secretion is normal.1 Thyroid nodules (TNs) are lesions that can arise as a consequence of localized abnormal thyroid cell proliferation. TNs are among the most common types of thyroid lesions, and TN incidence rates have risen to very high levels over the past three decades. A study has indicated that a TN prevalence rate of 68% in US.2 The most recent large-scale study conducted in 2021 estimated a TN prevalence rate of 36.9% in China.3 While the majority of these TNs are benign, an estimated 8–16% are malignant.4 While TNs do not cause notable clinical symptoms in most patients, their development is often related to various pathological thyroid conditions including autoimmune diseases, dysregulated endocrine function, and thyroiditis.5,6 Patients exhibiting symptomatic TNs generally undergo surgical resection, although this procedure can cause postoperative complications including hypothyroidism, infection, and damage to the laryngeal nerve.7 The effective treatment of TNs thus centers around the diagnosis and management of these nodules as early as possible in their development.
Many risk factors have been demonstrably linked to TN incidence, including both clinical and demographic characteristics. Both age and sex are related to TN prevalence among the residents of the USA, as are metabolic factors including female obesity, hypertension, diabetes, dyslipidemia, and fatty liver disease.8–10 Similar findings have also been reported in Chinese populations,6,11 with one study of 9898 individuals in Eastern China having demonstrated a link between metabolic disorders and elevated TN risk in both males and females.11 Other studies, however, have failed to detect any independent association between TN risk and either hyperuricemia or hyperlipidemia.12 As such, it remains controversial as to whether metabolic syndrome is an independent risk factor associated with TN incidence in China.
China is a large country that is home to populations of multiple ethnicities and a diverse range of environments such that risk factors are likely to vary substantially among regions. In southwest China, there have been few studies to date reporting on TN incidence. As such, the present study was conducted to explore the results of physical examinations performed in 45,023 adults conducted at a hospital in Luzhou, China, over a three-year period with the goal of describing TN rates in this population and identifying factors associated with the risk of developing these nodules in order to provide a reference that can guide the prevention or treatment thereof.
Materials and Methods
Study Subjects
This retrospective cohort study enrolled healthy adults who had undergone physical examinations at the Health Management Center of the Affiliated Hospital of Southwest Medical University of China from January 2019 to December 2021. Eligible participants were individuals ≥18 years of age who underwent thyroid ultrasound and abdominal ultrasound scans. Participants were excluded if their data were derived from repeat examinations, they were pregnant or lactating females, they had any history of thyroid disease and had undergone thyroid surgery or pharmacological treatment, or they had been diagnosed with cancer or any other serious disease.
This study was approved by the Institutional Review Board and Ethics Committee of Affiliated Hospital of Southwest Medical University (NO.KY2023175). The need for individual consent was waived by the committee due to the retrospective character of the study. The study was conducted in accordance with the Helsinki Declaration, and patients’records were anonymized prior to analysis.
Methods
Anthropometric Analyses
Detailed physical examinations were performed for all participants, which included measurements of height and weight using a physical examination scale (HNH-219, Omron, Shenzhen, China). Moreover, waist circumference (WC) was measured to the nearest 0.1 cm horizontally on bare skin using a flexible measuring tape at a point midway between the inferior margin of the ribs and the superior border of the iliac crest. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured two times using an automatic blood pressure monitor (HBP-9020, Omron, Dalian, China) placed on the right upper arm after participants had been seated quietly for a minimum of 5 values, with the lower of these two values ultimately being reported. Body mass index (BMI) = weight (kg)/[height (m)]2.
Laboratory Assays
Samples of participant serum were collected via venipuncture from 08:00 to 10:00 following overnight fasting, and were used to analyze fasting blood glucose (FBG), triglycerides (TG), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and uric acid (UA) levels.
Thyroid and Abdominal Ultrasonography
Professional ultrasound technicians performed thyroid and abdominal ultrasonography via B-mode US imaging (M7, Mindray, Shenzhen, China). Nodule characteristics were recorded, including nodule size (length, width), shape (aspect ratio ≥1, aspect ratio <1), structure (cystic, cystic-solid, solid), location, echo (no echo, high echo, equal echo, low echo, shallow echo), edge (regular, irregular, extraglandular invasion) and calcification. TNs were diagnosed based on the Kwak-TIRADs criteria13 as Category 1 (normal thyroid without any apparent nodules), Category 2 (definite benign lesions including typical subacute thyroiditis, thyroid cysts, nodular goiter, and simple calcifications), Category 3 (potentially benign nodules not exhibiting signs of malignancy), Category 4 (suspected malignancies, subclassified into categories 4a, 4b, or 4c based on whether they exhibited 1, 2, or 3–4 signs of malignancy), or Category 5 (TNs exhibiting 5 malignant signs). The five potential US signs examined to assess TN malignancy included solid structure, irregular or lobulated margins, low or shallow echo, an aspect ratio ≥1, and the presence of microcalcifications.
Fatty liver was diagnosed as per the revised diagnostic and treatment guidelines established in 2010 by the Fatty Liver and Alcoholic Liver Disease group of the Hepatology branch of the Chinese Medical Association.14
Definition of Variables
With respect to TN status, a TI-RADs category 1 classification was considered indicative of the absence of TNs, while TI-RADS categories 2–5 were used to identify patients harboring TNs.
Hypertension was defined by the 2013 European Society of Hypertension (ESH) 2013 guidelines (SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg). In addition, individuals take any oral antihypertensive medications were considered hypertensive. Hyperglycemic patients were classified into prediabetic and diabetic individuals based on the 2020 Chinese Prevention and Treatment of Type 2 Diabetes guidelines.15 Prediabetes was defined by impaired fasting glucose (IFG) as evidenced by FPG >6.1mmol/L and <7.0mmol/L or impaired glucose tolerance (IGT) defined by 2 h postprandial blood glucose (PPG) in 75 g OGTT ≥ 7.8 and <11.0 mmol/L. Diabetes was defined by FPG ≥ 7.0 mmol/L or 2 h PPG in 75 g OGTT ≥ 11.1 mmol/L. Individuals with diabetes were both participants who met these criteria as well as any individuals using hypoglycemic medications. The guidelines of the Chinese Medical Diabetes Association were used when diagnosing metabolic syndrome,16 which was established by identifying participants meeting three or more of the following criteria: (1) overweight/obese (BMI ≥ 25 kg/m2). (2) FPG ≥ 6.1 mmol/l and/or 2 h PPG ≥ 7.8 mmol/L, (3) hypertensive (SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg and/or taking antihypertensive medications), (4) dyslipidemic (TG ≥ 1.7 mmol/l and/or HDL-C <0.9 mmol/l (male) or <1.0 mmol/l (female)). BMI was defined as being underweight (<18.5 kg/m2), normal weight (≥18.5 kg/m2 and <24.0 kg/m2), overweight (BMI ≥ 24 kg/m2 and <28 kg/m2), and obese (≥28 kg/m2). Central obesity was defined by a WC ≥90 cm for males and ≥80 cm for females. Hyperuricemia was defined by uric acid levels > 420 μmol/L for males and >360 μmol/L for females. Classes of dyslipidemia included hypercholesterolemia (≥5.2 mmol), hypertriglyceridemia (>1.7 mmol/L), high LDL-C (≥3.4mmol/L), and low HDL-C (<1.0 mmol/L).
Statistical Analysis
Results were analyzed with SPSS v 17.0 (IBM Corporation, NY, USA). Continuous data are reported as means ± standard deviation, and categorical data are given as frequencies with percentages. These results were compared using t-tests or chi-square tests. Additionally, univariate and multivariate logistic regression analyses were conducted and utilized to compute odds ratios (ORs) and 95% confidence intervals (CIs) with the goal of identifying risk factors associated with TN development, with a two-sided P < 0.05 as the significance threshold.
Results
Participant Characteristics
In total, this study incorporated 45,023 healthy adults, including 21,108 men (46.88%) and 23,915 women (53.12%). These individuals were a mean of 42.05±12.41 years of age, with a mean BMI of 23.50±3.37 kg/m2, a mean waist circumference of 79.64±10.17 cm, a mean systolic blood pressure of 118.44±16.23 mmHg, mean diastolic blood pressure of 72.29±10.82 mmHg, a mean fasting plasma glucose was 5.11±1.21 mmol/L, a mean total cholesterol level of 4.76±0.91 mmol/L, a mean triglyceride level of 1.59±1.54 mmol/L, a mean HDL level of 1.38±0.36 mmol/L, a mean LDL level of 2.92±0.85 mmol/L, and a mean uric acid level of 344.16±93.06 μmol/L. Of these participants, 13,566 (30.13%) exhibited fatty liver (Table 1).
 |
Table 1 Baseline Participant Characteristics (n = 45,023) |
TN Detection Rates
TNs were detected in 29.8% of these participants, including 23.2% of men and 35.7% of women. Relative to individuals without TNs, the average age of individuals with TNs at the time of examination was significantly higher (39.98±11.74 vs 46.93±12.57; t = −56.295, P < 0.001), and there was a significant difference in the TN detection rate among age groups (χ2=2870.057, P < 0.001, Table 1), with a chi-square trend test indicating that this detection rate rose with age (χ2=2775.661, P < 0.001) (Figure 1).
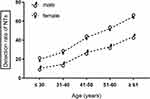 |
Figure 1 Trends in TN detection as a function of age and gender. |
Univariate Analysis Results
Univariate analyses revealed that factors positively associated with the risk of TN development included BMI, central obesity, hypertension, IFG, DM, metabolic syndrome, hypercholesterolemia, high LDL-C, and fatty liver, whereas factors negatively associated with TN development included low HDL-C and hyperuricemia (P < 0.01; Table 2). When participants were analyzed by gender, low HDL-C and hypertriglyceridemia were found to be unrelated to TN risk in men (P > 0.05; Table 2), whereas in women low HDL-C levels were unrelated to TN risk (P > 0.05; Table 2), and both hypertriglyceridemia and hyperuricemia were positively related to TN risk (P < 0.01; Table 2).
 |
Table 2 Univariate Analyses of Factors Associated with TN Risk (n = 45,023) |
Multivariate Logistic Regression Analysis Results
To better identify risk factors related to TN development, significant variables identified in the above univariate analyses were next subjected to multivariate logistic regression analysis. In the overall patient population, impaired fasting glucose (OR = 1.194, 95% CI:1.065–1.340) was related to an elevated risk of TN development. Females faced a 2.283-fold higher risk of TNs relative to males (OR = 2.283, 95% CI:2.177–2.393). The risk of TNs also rose with age such that relative to individuals ≤30 years old, individuals from 31 to 40 (OR = 1.469, 95% CI:1.368–1.576), 41–50 (OR = 2.931, 95% CI:2.734–3.142), 51–60 (OR = 4.060, 95% CI:3.773–4.369), and ≥61 (OR = 6.487, 95% CI:5.893–7.140) were all at a higher risk of TN development. Moreover, this risk was increased in those exhibiting central obesity (OR = 1.115, 95% CI:1.051–1.183) and in both overweight (OR = 1.085, 95% CI:1.026–1.147) and obese (OR = 1.156, 95% CI:1.054–1.268) individuals relative to those of normal weight (Figure 2). Lower BMI values were associated with reduced TN risk (OR = 0.789, 95% CI:0.706–0.882) (Figure 2). When participants were separated into gender-based subgroups, impaired fasting glucose did not remain an independent predictor of risk among males (Figure 3), whereas high LDL-C levels were an independent protective factor among females, and no other indicators exhibited any significant changes (Figure 4).
 |
Figure 3 Independent risk factors associated with TNs in males identified through a multivariate binary logistic regression analysis. Abbreviation: BMI, body mass index. |
Discussion
Changing lifestyle factors, rising rates of ultrasonographic scanning, and other detection strategies have all contributed to rising rates of TN detection in China and throughout the globe. However, no epidemiological studies of TN incidence have been conducted at the nationwide level in China to date, and those studies that have been performed have revealed differences in TN prevalence across specific regions (East China 50.2%, Chongqing 34.1%, Beijing 36.3%).11,12,17 Comparable studies conducted in Southwest China have been lacking, and this large-scale retrospective cohort study was thus used to assess TN incidence rates and associated risk factors in the Chinese population. Data were analyzed for 45,024 adults who underwent physical examinations in a Grade A hospital, revealing a TN detection rate of 29.8% (23.2% in men and 35.7% in women). This rate is slightly below previously reported rates. This may be attributable to the fact that these study participants were individuals undergoing physical examinations in the Southwest provinces of China (Yunnan, Guizhou, Sichuan), with a wide range of participant ages (18–95 years old) such that 49.16% were under the age of 40, which is noteworthy given that TN detection rates in young individuals are low. Second, Southwest China is an area with low iodine content in water. Residents use iodized salt to ensure good iodine intake.18 So the iodine intake of individuals in Southwest China is generally good, and few TNs resulting from iodine deficiency thus develop in this region. Moreover, a higher risk of TN development was observed among females in every age group, consistent with the results of other studies.
After an initial ultrasound (US), the next step in assessing the risk of cancer of a thyroid lesion is fine needle aspiration (FNA). The accepted method for analyzing FNA cytology is the Bethesda categorization system. Heterotypic/follicular lesions of unknown significance (AUS/FLUS), commonly referred to as Bethesda III, are the most controversial category due to their heterogeneity and inconsistent reporting. The total risk of cancer for thyroid nodules in Bethesda classifications III–IV is between 15% and 40%.19 In addition, thyroid nodules in Bethesda II also have an incidental cancer risk of 1.53%.20
A complex series of factors including age, gender, and iodine intake can all influence TN development. Moreover, metabolic syndrome has been established as being independently associated with TN risk.8 Here, age, gender, BMI, central obesity, and blood glucose levels were all found to be significantly related to TN development in this population of individuals undergoing physical examinations.
Age can have a major impact on TN incidence rates. As humans age, the production of reactive oxygen species and free radicals becomes enhanced, causing harm to cells that can contribute to cellular damage and changes in thyroid tissue including fibrosis and aging, eventually leading to TN formation.21 When participants were stratified based on age, higher age was linked to an elevated risk of TNs. This remained true following gender-based patient stratification. Prior evidence indicated that females were at a higher risk of TN development relative to males,3,9,11 with a 2.8-fold higher risk of TNs in this study cohort. Another report highlighting increased TN rates among females suggested that these rates are associated with estrogen and progesterone levels.22 Kung et al23 determined that pregnancy was related to the odds of TN development and to the enlargement of preexisting TNs.
In the present study, both central obesity and a BMI classified as overweight/obese were independently associated with the risk of TN development. The association between obesity and TNs may be related to adipose tissue-mediated leptin secretion. As BMI and leptin levels are positively correlated,24 this may explain the rising TSH levels observed as BMI increases. Generally, obese people have leptin resistance, leading to an increase in plasma leptin concentration. Excessive leptin can promote autoimmune thyroid disease, and can also up-regulate the hypothalamus-pituitary-thyroid axis, leading to hyperthyrotropism.25 Specifically, elevated levels of leptin in the serum of obese individuals can promote higher levels of TSH, which in turn drive TN development. One study consistently found BMI to be positively correlated with TN incidence.26 Xu et al27 separated study subjects into two groups based upon whether or not their BMI was below 24 kg/m2, revealing that a BMI ≥ 24 kg/m2 was significantly correlated with a higher risk of TN incidence, in line with the present results. Moreover, BMI < 18.5 was herein found to be protective against TN development among healthy individuals, suggesting that underweight individuals are less likely to exhibit TNs. This may be related to levels of TSH and other hormones, although future prospective cohort study-based validation of these findings will be essential. Central obesity was herein identified as a factor independently related to TN risk, and this remained true even when analyzing gender-based subgroups. Central obesity has already been shown to be associated with a higher risk of adverse metabolic health outcomes,28,29 including hyperglycemia, hypertension, and dyslipidemia, reflecting a range of components of metabolic syndrome. Central obesity is a core component of this metabolic syndrome.30 Song et al31 reported that WC was superior to BMI when evaluating patient TN risk, and in the present study the value of these predictors remained consistent following gender-based stratification.
In this study, IFG was associated with TN development such that prediabetic individuals were at a higher risk of TN incidence. In a study conducted by Anil et al32 in Turkey, larger thyroid size and higher rates of TN development were observed in individuals suffering from impaired glucose metabolism. Rezzonico et al33 found metformin to produce significant reductions in nodular size in individuals exhibiting insulin resistance harboring small TNs. Abnormal glucose metabolism can alter the energy metabolism of thyroid follicular cells, thus promoting TN development. When participants were analyzed based on gender, significant correlations were detected between age, BMI, central obesity, and TN incidence for both males and females. Impaired fasting glucose was also related to TN incidence among women. Prior research has indicated that TG levels are related to diabetic onset,34,35 and Winzer et al36 demonstrated that women exhibited higher levels of blood lipids relative to age-matched men following menopause, significantly impacting TG levels. This suggests that blood lipid levels can be impacted by estrogen. While high TG levels were herein found to be related to TN incidence in women, the same was not true in men.
Here, blood pressure, uric acid levels, and dyslipidemia (TG, RC, HDL, and LDL) were all found to be significantly associated with nodular disease. However, these factors were ultimately not identified as being risk factors independently associated with TN incidence in contrast to some prior evidence.3,37,38 For example, Zou et al39 reported higher LDL-C levels to be more closely associated with multiple thyroid sarcoidosis, while Liu et al38 identified uric acid levels as being protective in men over the age of 30 yet a risk factor in both women older than 30 and men younger than 30. When specifically evaluating patient subgroups based on gender, high LDL-C levels were identified as a protective factor in females. As such, the precise role that hypertension, uric acid levels, and serum lipids play in the promotion of TN development remains to be fully clarified. Differences among studies and subgroups may be attributable to differences in the enrolled subjects and to limited sample sizes. Additional prospective cohort studies should be conducted to better clarify how lipid levels and uric acid influence TN risk.
Newly discovered NTs in potential organ donors need to be investigated to rule out cancer and avert any subsequent risk of transmission.40 However, there are no established protocols that clearly address the management of thyroid nodules in deceased donors for transplantation.41 Our findings have some significance in the context of the donor population. This study provides a new approach to assessing the risk of TNs through risk factors and valuable data for preliminary assessment of the risk TNs in donors. That is to say, and for donors who do not know if they have thyroid nodules, somebody can evaluate through risk factors.
While the present study compiles large quantities of data from a large patient population and will thus serve as a valuable reference resource, it is nonetheless subject to certain limitations. Notably, factors such as participant diet, education levels, lifestyle factors, and economic status were not taken into account.
Conclusion
In most cases, TNs do not exhibit any overt symptoms during their early stages, and as such, thyroid ultrasonography and thyroid function tests can aid in the early detection of these nodules. For women aged ≥31 years old, individuals who are overweight/obese, and those with high blood glucose levels, thyroid ultrasound screening should be recommended to facilitate early detection and diagnosis. In addition, healthy individuals should engage in primary preventative measures aimed at reducing TN incidence through lifestyle adjustments and the control of body mass, while individuals already suffering from metabolic diseases should actively seek to regulate their blood glucose levels.
Acknowledgments
This study was supported in part by Grants from the key research base of Science and Technology Research Fund Project of Luzhou city (2021-SYF-36), the Scientific Research Fund project of Southwest Medical University (2020ZRQNB027). They thank all study participants and staff members who assisted with this analysis.
Disclosure
The authors declare that there are no conflicts of interest regarding the publication of this paper.
References
1. Francesk M, Anjum F. Thyroid Adenoma. In: StatPearls. StatPearls Publishing; 2023.
2. Kuo JH, McManus C, Lee JA. Analyzing the adoption of radiofrequency ablation of thyroid nodules using the diffusion of innovations theory: understanding where we are in the United States? Ultrasonography. 2022;41(1):25–33. doi:10.14366/usg.21117
3. Li Y, Jin C, Li J, et al. Prevalence of thyroid nodules in china: a health examination cohort-based study. Front Endocrinol. 2021;2021:9.
4. Burman KD, Wartofsky L. Clinical practice. Thyroid nodules. N Engl J Med. 2015;373(24):2347–2356. doi:10.1056/NEJMcp1415786
5. Canete EJ, Sison-Pena CM, Jimeno CA. Clinicopathological, biochemical, and sonographic features of thyroid nodule predictive of malignancy among adult Filipino patients in a tertiary hospital in the Philippines. Endocrinol Metab. 2014;29(4):489–497. doi:10.3803/EnM.2014.29.4.489
6. Zheng L, Yan W, Kong Y, et al. An epidemiological study of risk factors of thyroid nodule and goiter in Chinese women. Int J Environ Res Public Health. 2015;12(9):11608–11620. doi:10.3390/ijerph120911608
7. Sosa JA, Bowman HM, Tielsch JM, et al. The importance of surgeon experience for clinical and economic outcomes from thyroidectomy. Ann Surg. 1998;228(3):320–330. doi:10.1097/00000658-199809000-00005
8. Kim JY, Jung EJ, Park ST, et al. Body size and thyroid nodules in a healthy Korean population. J Korean Surg Soc. 2012;82(1):13–17. doi:10.4174/jkss.2012.82.1.13
9. Moon JH, Hyun MK, Lee JY, et al. Prevalence of thyroid nodules and their associated clinical parameters: a large-scale, multicenter-based health checkup study. Korean J Intern Med. 2018;33(4):753–762. doi:10.3904/kjim.2015.273
10. Simsir IY, Cetinkalp S, Kabalak T. Review of factors contributing to nodular goiter and thyroid carcinoma. Med Princ Pract. 2020;29(1):1–5. doi:10.1159/000503575
11. Chen Y, Zhu C, Chen Y, et al. The association of thyroid nodules with metabolic status: a cross-sectional SPECT-China study. Int J Endocrinol. 2018;2018:8. doi:10.1155/2018/6853617
12. Xu L, Zeng F, Wang Y, et al. Prevalence and associated metabolic factors for thyroid nodules: a cross-sectional study in Southwest of China with more than 120 thousand populations. BMC Endocr Disord. 2021;21(1):11. doi:10.1186/s12902-021-00842-2
13. Park JY, Lee HJ, Jang HW, et al. A proposal for a thyroid imaging reporting and data system for ultrasound features of thyroid carcinoma. Thyroid. 2009;19(11):1257–1264. doi:10.1089/thy.2008.0021
14. Fatty liver and alcoholic liver disease group. Hepatology branch, Chinese medical association, “guidelines for the diagnosis and treatment of nonalcoholic fatty liver disease (revised in 2010). Chin J Hepatol. 2010;19(6):483–487.
15. Diabetes branch of Chinese Medical Association. Chinese guidelines for the prevention and treatment of type 2 diabetes (2020 Edition). Chin J Diabetes Mellitus. 2021;13(4):315–409.
16. Lu Y, Lu J, Wang S, et al. Comparative analysis of diagnostic criteria of metabolic syndrome between International Diabetes Federation and Chinese Diabetes Association. Natl Med J China. 2006;86(6):386–389.
17. Li Y, Xiao Z. Detection rate and characteristic analysis of thyroid nodules in health examination patients. Chin J Clin. 2015;43(6):54–55.
18. Teng WP, Liu K. Adhere to salt iodization to protect thyroid health -- Interpretation of the results of the national iodine nutrition and thyroid disease survey. China Med News. 2020;35(19):18.
19. Francesk M, Plachouri MK, Liolis E, et al. Patient outcomes following surgical management of thyroid nodules classified as Bethesda category III (AUS/FLUS). Endokrynol Pol. 2021;72(2):143–144. doi:10.5603/EP.a2021.0018
20. Francesk M, Iliopoulos F, Tsilivigkos C, et al. Cancer rate of Bethesda category II thyroid nodules”, Medicinski glasnik: official publication of the Medical Association of Zenica-Doboj Canton. Bosnia Herzegovina. 2022;19:1.
21. Su Y, Zhang Y, Zhao M, et al. Association between thyroid nodules and volume and metabolic syndrome in an iodine-adequate area: a large community-based population study. Metab Syndr Relat Disord. 2019;17(4):217–222. doi:10.1089/met.2018.0094
22. Dauksiene D, Petkeviciene J, Klumbiene J, et al. Factors associated with the prevalence of thyroid nodules and goiter in middle-aged euthyroid subjects. Int J Endocrinol. 2017;2017:8. doi:10.1155/2017/8401518
23. Kung AWC, Chau MT, Lao TT, et al. The effect of pregnancy on thyroid nodule formation. J Clin Endocrinol Metab. 2002;87(3):1010–1014. doi:10.1210/jcem.87.3.8285
24. Paul RF, Hassan M, Nazar HS, et al. Effect of body mass index on serum leptin levels. J Ayub Med Coll Abbottabad. 2011;23(3):40–43.
25. Gar C, Rottenkolber M, Haenelt M, et al. Altered metabolic and hormonal responses to moderate exercise in overweight/obesity. Metabolism. 2020;107:154219. doi:10.1016/j.metabol.2020.154219
26. Jin JR, Machekano R, McHenry CR. The utility of preoperative serum thyroid-stimulating hormone level for predicting malignant nodular thyroid disease. Am J Surg. 2010;199(3):294–298. doi:10.1016/j.amjsurg.2009.08.028
27. Xu W, Chen Z, Li N, et al. Relationship of anthropometric measurements to thyroid nodules in a Chinese population. BMJ Open. 2015;5(12):10. doi:10.1136/bmjopen-2015-008452
28. Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr. 2004;79(3):379–384. doi:10.1093/ajcn/79.3.379
29. Zhang P, Wang R, Gao C, et al. Prevalence of central obesity among adults with normal BMI and its association with metabolic diseases in Northeast China. PLoS One. 2016;11:7.
30. Alberti KG, Zimmet P, Shaw J. The metabolic syndrome--a new worldwide definition. Lancet. 2005;366(9491):1059–1062. doi:10.1016/S0140-6736(05)67402-8
31. Song B, Zuo Z, Tan J, et al. Association of thyroid nodules with adiposity: a community-based cross-sectional study in China. BMC Endocr Disord. 2018;18(1):8. doi:10.1186/s12902-018-0232-8
32. Anil C, Akkurt A, Ayturk S, et al. Impaired glucose metabolism is a risk factor for increased thyroid volume and nodule prevalence in a mild-to-moderate iodine-deficient area. Metabolism. 2013;62(7):970–975. doi:10.1016/j.metabol.2013.01.009
33. Rezzonico J, Rezzo’nico M, Pusiol E, et al. Metformin treatment for small benign thyroid nodules in patients with insulin resistance. Metab Syndr Relat Disord. 2011;9(1):69–75. doi:10.1089/met.2010.0026
34. Kahn HS, Cheng YJ, Thompson TJ, et al. Two risk-scoring systems for predicting incident diabetes mellitus in U.S. adults age 45 to 64 years. Ann Intern Med. 2009;150(11):741–751. doi:10.7326/0003-4819-150-11-200906020-00002
35. Wang W, Liu J, Sun J, et al. A cohort study of triglyceride levels and the risk of diabetes onset. Chin J Intern Med. 2012;51(7):516–519.
36. Winzer C, Wagner O, Festa A, et al. Plasma adiponectin, insulin sensitivity, and subclinical inflammation in women with prior gestational diabetes mellitus. Diabet Care. 2004;27(7):1721–1727. doi:10.2337/diacare.27.7.1721
37. Yin J, Wang C, Shao Q, et al. Relationship between the prevalence of thyroid nodules and metabolic syndrome in the iodine-adequate area of Hangzhou, China: a cross-sectional and cohort study. Int J Endocrinol. 2014;2014:7. doi:10.1155/2014/675796
38. Liu Y, Lin Z, Sheng C, et al. The prevalence of thyroid nodules in northwest China and its correlation with metabolic parameters and uric acid. Oncotarget. 2017;8(25):41555–41562. doi:10.18632/oncotarget.14720
39. Zou B, Sun L, Wang X, et al. The prevalence of single and multiple thyroid nodules and its association with metabolic diseases in Chinese: a cross-sectional study. Int J Endocrinol. 2020;2020:11. doi:10.1155/2020/5381012
40. Ammendola S, Girolami I, Bovo C, et al. Thyroid fine-needle aspiration cytology: focusing on adherence to guidelines and hospital organization. Am J Case Rep. 2020;21:1. doi:10.12659/AJCR.920933
41. Eccher A, Girolami I, D’Errico A, et al. Management of thyroid nodules in deceased donors with comparison between fine needle aspiration and intraoperative frozen section in the setting of transplantation. Prog Transplant. 2019;29(4):316–320. doi:10.1177/1526924819873898
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


