Back to Journals » Integrated Blood Pressure Control » Volume 16
High Prevalence of Uncontrolled Hypertension Among Afghan Hypertensive Patients: A Multicenter Cross-Sectional Study
Authors Baray AH, Stanikzai MH , Wafa MH , Akbari K
Received 14 April 2023
Accepted for publication 29 June 2023
Published 4 July 2023 Volume 2023:16 Pages 23—35
DOI https://doi.org/10.2147/IBPC.S417205
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Konstantinos Tziomalos
Ahmad Haroon Baray,1 Muhammad Haroon Stanikzai,1 Mohammad Hashim Wafa,2 Khalid Akbari3
1Department of Public Health, Faculty of Medicine, Kandahar University, Kandahar, Afghanistan; 2Neuropsychiatric and Behavioral Science Department, Faculty of Medicine, Kandahar University, Kandahar, Afghanistan; 3Internal Medicine Department, Faculty of Medicine, Paktia University, Paktia, Afghanistan
Correspondence: Muhammad Haroon Stanikzai, Department of Public Health, Faculty of Medicine, Kandahar University, District # 10, Kandahar, Afghanistan, Tel +93704775578, Email [email protected]
Background: Despite striking advances in the management of hypertension, blood pressure (BP) control remains suboptimal worldwide. Sustainable Development Goals (SDGs) call for 80% control rates by 2030, highlighting the urgency for improvements in hypertension control.
Objective: We aimed to determine the prevalence of uncontrolled hypertension (≥ 140/90 mmHg) and assess its associated factors in Afghan hypertensive patients.
Methods: We conducted this multicenter cross-sectional study at three Afghan public hospitals in Afghanistan. We recruited hypertensive patients (n=950) on antihypertensive medications (AHMs) from August to December 2022. We analyzed only complete datasets (853). We employed the 14-item Hill-Bone compliance scale to assess compliance with AHMs. We performed multivariable logistic regression analyses to determine factors associated with uncontrolled hypertension.
Results: The mean age (±SD) of the patients was 47.5 (± 9.5) years and males constituted 50.5% (431) of the study sample. The prevalence of uncontrolled hypertension in this study was 77.3% (95% CI: 74.2– 79.9%). Factors associated with uncontrolled hypertension and their adjusted OR (95% CI) were physical inactivity: 3.45 (1.87– 6.35), current smoking: 3.04 (1.50– 6.15), high salt intake: 3.57 (1.9– 6.7), presence of comorbid medical disease: 2.22 (1.20– 4.08), higher BMI: 3.32 (1.12– 9.88), poor compliance to AHMs: 8.50 (4.62– 15.6), and presence of depressive symptoms: 1.99 (1.2– 3.27).
Conclusion: The prevalence of uncontrolled hypertension was high in the present study. Factors associated with uncontrolled hypertension may epitomize potential targets for public/individual health interventions in Afghanistan.
Keywords: hypertension, uncontrolled, prevalence, risk factors, Afghanistan
Introduction
Uncontrolled hypertension is unacceptably high in low- and middle-income countries (LMICs).1 A growing body of knowledge indicates that uncontrolled hypertension results in higher rates of premature cardiovascular diseases and deaths.1,2 Despite striking advances in the management of hypertension, blood pressure (BP) control remains suboptimal worldwide.1,2 Sustainable Development Goals (SDGs)call for 80% control rates by 2030, highlighting the urgent need for improvements in hypertension control.3 Effective, safe, and efficient interventions can significantly decrease hypertension-related morbidity and mortality rates in LMICs.1,4
Globally, 31.1% (1.13 billion) of adults aged 30–79 years had hypertension in 2015, of which 79% had uncontrolled hypertension.1,5 Studies across regions have reported that the prevalence of hypertension ranges from 28.5% in high-income countries to 31.5% in middle and low-income countries.5 In Afghanistan, hypertension affects approximately 30% (5.3 million) of the adult population, and the prevalence of uncontrolled hypertension is approximately 80% (4.2 million).6 The actual estimates of uncontrolled hypertension may be higher due to the under-reporting of cases in developing countries, especially Afghanistan. The need for improvements in hypertension control is particularly urgent in Afghanistan, where uncontrolled hypertension continues to be a major public health issue.7
Medical, social, and economic costs associated with uncontrolled hypertension are high.1,2 Patients with uncontrolled hypertension develop cardiovascular, renal, and cerebrovascular morbidity and mortality.1,2 In addition, their quality of life is strongly affected by their physical and psychological disabilities.8,9 As a result, poor quality of life can adversely affect adherence to antihypertensive medications (AHMs).9 Additionally, the economic burden of hypertension is a leading public health challenge in developing countries.10,11
In Afghanistan, hypertension is among the top ten causes of death.12 A previous study showed that in Afghanistan, the prevalence of uncontrolled hypertension was 75% and staggered in the adult population, causing cardiovascular diseases with substantial morbidity and mortality in patients with hypertension.13 Various studies have revealed that poor hypertension control in developing countries is due to many reasons, such as poor adherence to AHMs, clinical inertia, mental health conditions, lack of free or low-cost BP medicines, physical inactivity, non-adherence to low salt intake, failure to focus better on social determinants of health, accessibility of healthcare facilities, and organizational failure.13–17 However, there is limited evidence in the study area regarding uncontrolled hypertension and its associated factors in patients receiving treatment. Therefore, this study aimed to determine the prevalence of uncontrolled hypertension and assess the factors associated with poor hypertension control in three public hospitals across Afghanistan.
Materials and Methods
Study Settings and Design
This cross-sectional study included adults with hypertension at public hospitals in Afghanistan. We conducted this study at three public hospitals in Afghanistan between August and December 2022. The three study sites were Mirwais Regional Hospital in Kandahar, Ibn Sina Hospital in Kabul, and the Paktia Provincial Hospital in Paktia. Each hospital has a designated outpatient department for internal medicine, which delivers diagnostic and therapeutic services for patients with hypertension, Diabetes Mellitus (DM), and other common medical conditions. The study sites were selected through convenience sampling.
Sample Size and Sampling
To calculate our sample size of 850 participants, we employed a single population proportion formula considering the prevalence of uncontrolled hypertension at 75%, 5% margin of error, a 95% confidence interval, and a 10% non-response rate. A design effect of 2.0 was included which doubled the required sample size. There were a total of 2523 hypertensive patients on initial visit in three hospitals: Mirwais Regional hospital (1012), Ibni Sina Hospital (780), and Paktia Provincial Hospital (731). The sample population was distributed among the three hospitals using a systematic sampling method. We randomly recruited 950 hypertensive patients at their initial visit to three public hospitals and at the three-month follow-up visit. The response rate was 90.7% (n = 862). The final analysis consisted of 853 (89.7%) participants with complete datasets. Finally, 395, 243, and 215 hypertensive patients were selected from Mirwais Regional Hospital, Ibni Sina Hospital, and Paktia Provincial Hospital, respectively.
Study Population
We included all consenting adult (≥ 18 years old) hypertensive patients receiving antihypertensive follow-up treatment at public hospitals for at least three months at the time of our data collection. We excluded pregnant women, patients with compromised consciousness, and those diagnosed with hypertensive urgency or emergency conditions. Moreover, we excluded patients with missing blood pressure data or other related variables (Figure 1).
 |
Figure 1 Participants’ inclusion flow chart. |
Study Variables
Dependent Variable
Uncontrolled hypertension is a systolic blood pressure ≥ 140 mmHg and a diastolic blood pressure ≥ 90 mmHg, despite medical treatment.18 It was the dependent variable. We followed the guidelines of the American Heart Association for blood pressure measurements.19 To measure BP, the investigators used a manual sphygmomanometer. We calculated the mean of three BP measurements.
Independent Variables
The socio-demographics of our participants included age, sex, residence, marital status, educational background, occupation, monthly household income, and Body Mass Index (BMI).
Lifestyle/behavior-related variables included smoking, physical activity, and treatment adherence. Other variables of interest included table-added salt and fruit and vegetable intake. The presence of concomitant medical conditions, family history of hypertension, duration of hypertension, and antihypertensive medications were health-related characteristics of the patients.
In this study, we employed a validated International Physical Activity Questionnaire (IPAQ) to measure the level of physical activity among the study participants.20,21 Additionally, we employed the term pre-existing comorbidity to denote a chronic health problem, such as Ischemic Heart Disease (IHD), Diabetes Mellitus (DM), and chronic kidney diseases that the patient might have along with hypertension.
This study employed the 14-item version of the Hill-Bone compliance scale to assess compliance with high blood pressure treatment.22,23 The compliance scale measures three important behavioral domains of high blood pressure treatment: appointment keeping (3 items), diet (2 items), and medication adherence (9 items). The Hill-Bone compliance scale is a globally credible instrument with good internal validity and reliability for assessing compliance with high blood pressure treatment.22–24
We employed the Patient Health Questionnaire-9 (PHQ-9) to measure the presence and severity of depressive symptoms during the last two weeks and assess the prevalence of probable depression. The PHQ-9 is a 4-point scale from 0 (not at all) to 3 (nearly every day), yielding a total score from 0 to 27. The questionnaire is a globally credible instrument with good psychometric properties for assessing depressive symptoms based on DSM-IV criteria.25,26 The internal consistency (Cronbach’s alpha) value for the Pashtu version in this study was 0.92.
Data Collection
The study questionnaire was initially drafted in English language and then translated into the local languages (Pashtu and Dari) spoken by the study participants. Bilingual translators familiar with the medical terminology used in the questionnaire translated the questionnaire. We assessed the clarity and simplicity of the final version of the questionnaire through a pilot study of a small group of teaching hospital patients at Kandahar University. Patients who consented to the pilot study had socio-demographic attributes (eg, age, sex, and education level) similar to those of the study population. We employed the pilot study results to refine the questionnaire for its cultural appropriateness and linguistic accuracy for the target population.
A team of six trained medical doctors and three supervisors (trainees of the Master of Public Health Program) collected the data. The data collection process followed standard protocols and ethical guidelines to ensure the privacy and confidentiality of the study participants. We designed the data collection process to minimize any potential bias or errors that could affect the accuracy and reliability of the collected data. Additionally, the collected data were regularly reviewed and monitored to ensure that the data met the required quality standards for analysis and interpretation.
Statistical Analysis
We used the Statistical Package for Social Sciences (SPSS) version 21.00 for data analysis.27 We conducted descriptive statistics, such as mean, standard deviation, frequency, and percentage, to understand the participants’ socio-demographics, lifestyle, and other related characteristics. Based on the literature review, we employed inferential statistics, such as chi-square tests, to investigate the association of potential factors with poor BP control. Independent variables evaluated included: socio-demographics, lifestyle/behavioral, and other related characteristics of the patients. We identified and retained every independent variable with a p-value < 0.25 in the multivariable logistic regression. After adjusting for age and gender, we performed multivariable logistic regression to determine the factors associated with uncontrolled hypertension in our subjects. We set statistical significance at P < 0.05.
Results
We interviewed 853 hypertensive patients from the 950 recruited patients, yielding a response rate of (89.7%). In our sample, 50.5% (431) were males, and the mean age (±SD) of the patients was 47.5 (± 9.5) years. A big chunk (777; 91.1%) of our participants were married, and more than two-thirds (584; 68.5%) had no formal education. Approximately one-third (35.8%) of the patients were gainfully employed, and the median household monthly income was Afghanis 9000 (IQR: 6000–13,000), which is equivalent to approximately USDS 105 (March 2023). Their BMI was 23.3 Kg/m2, and less than a fourth of our participants (195; 22.9%) were overweight or obese. Table 1 illustrates the detailed socio-demographics of the patients.
 |
Table 1 Socio-Demographic Characteristics of the Study Participants (n=853) |
Table 2 summarizes the behavioral and lifestyle characteristics of the study participants. About 28.7% (245) of the study participants were current smokers, and 80.2% (684) were physically inactive. Only 12.2% (76) and 11% (94) of the patients consumed fresh fruits and vegetables more often (daily), respectively. One-third (33.1%, 282) of the participants reported adding salt to their food at the table (Table 2).
 |
Table 2 Behavioral/Lifestyle Characteristics of the Study Participants (n=853) |
The mean duration (±SD) of hypertension was 6.8 (± 5.06) years (range 1–45 years), and 48.7% (415) had a family history of hypertension. Of all respondents, 38.5% (328) had comorbid medical disease, 30.2% (258) were using NSAIDs, and 23.9% (204) reported BP monitoring at home. More than a fourth (230; 27.0%) were taking one type of AHM, 290 (34%) were taking two types of AHMs, and 333 (39%) were taking three or more types of AHMs. Approximately 30% (256) of the patients reported traditional approaches to treating their hypertension. A significant proportion of patients (91.1%, 777) used to buy their AHMs from private pharmacies. The prevalence of depressive symptoms was 51.8%, with mild, moderate, moderately severe, and severe depression categories at 10.9%, 27.4%, 13.0%, and 0.5%, respectively. The mean compliance score (±SD) using the Hill Bone antihypertensive compliance scale was 23.6 (± 3.5) and 42.1% (359) had poor compliance (lowest score of 14 indicates good compliance, highest score 56 indicates poor compliance) (Table 3).
 |
Table 3 Health Profile Related Characteristics of the Study Participants (n=853) |
At the time of this study, we found that the prevalence of uncontrolled hypertension was 77.3% (95% CI: 74.2–79.9%) among our study participants (Figure 2).
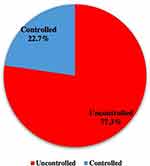 |
Figure 2 Prevalence of uncontrolled hypertension among study participants (n=853). |
Factors Associated with Uncontrolled Hypertension Among Study Participants
A multivariable logistic regression analysis indicated that physical inactivity (AOR= 3.45, 95% CI: 1.87–6.35), smoking (AOR= 3.04, 95% CI: 1.50–6.15), high salt intake (AOR= 3.57, 95% CI: 1.9–6.7), presence of comorbid medical disease (AOR= 2.22, 95% CI: 1.20–4.08), higher BMI (AOR= 3.32, 95% CI: 1.12–9.88), poor compliance to AHMs (AOR= 8.50, 95% CI: 4.62–15.6), and presence of depressive symptoms (AOR= 1.99, 95% CI: 1.2–3.27) were factors associated with uncontrolled hypertension (Table 4).
 |
Table 4 Factors Associated with Uncontrolled Hypertension; Crude and Adjusted Odds Ratio with 95% CI |
Discussion
In this study of 853 adult patients with hypertension, we found that 77.3% had uncontrolled hypertension. Multivariable analyses showed that several patient attributes (ie, physical activity, smoking status, salt intake, BMI, presence of medical comorbidities and depressive symptoms, and compliance with AHMs) were significantly associated with uncontrolled hypertension.
In the present study, the vast majority (77.3%) of the patients had uncontrolled hypertension during their follow-up visit at public hospitals. Previous studies on LMICs have found that the prevalence of uncontrolled hypertension varies substantially from country to country and even by region within a country. For instance, a recent systematic review and meta-analysis of community based non-interventional studies from India found that the pooled prevalence of uncontrolled hyperextension was as high as 82.5% and had significantly poor control rates in the eastern region.17 Findings from several other LMICs reported uncontrolled hypertension in 82.5% of the study participants in Uganda,28 and 52.1% in Ethiopia.14 Variation in the prevalence of uncontrolled hypertension reported in pertinent literatures can be attributed to variation in socioeconomic status, geographic locations, research methodology, dietary habits of study participants, and other non-explored factors. These considerably high rates of uncontrolled hypertension emphasize the necessity for perpetual monitoring and improved management of hypertension, particularly in Afghanistan, where access to healthcare services and medications is limited.7
In this study, physically inactive patients suffered from uncontrolled hypertension, supporting the previously published findings that physically inactive patients with hypertension are more likely to have uncontrolled hypertension.17,28 Furthermore, our results showed that high BMI (overweight/ obesity) also played a significant role in uncontrolled hypertension. These findings highlight the need to promote physical activity in the Afghan population to enhance the prevention and management of hypertension. Thus, addressing physical inactivity and encouraging regular exercise may improve overall health by ensuring appropriate body weight and lowering the risk of other chronic diseases, such as type 2 diabetes and certain types of cancer.29,30
Our findings indicate that current smoking was associated with uncontrolled hypertension. This result is consistent with other pertinent studies, for instance, the Hypertension Optimal Treatment (HOT) study that has also observed high rates of uncontrolled hypertension in current smokers.31 Notably, recent studies have demonstrated the role of smoking cessation in reducing cardiovascular complications in high-risk populations.14,32 Hence, developing and implementing smoking cessation strategies specific to patients with hypertension are crucial.
We observed that our subjects with added table salt were more likely to report higher rates of uncontrolled hypertension than their counterparts. Consistently, extensive evidence has shown that high salt intake increases the rate of uncontrolled hypertension and that dietary salt restriction leads to a better response to AHMs.33,34 The higher levels of hypertension among patients with high salt intake result from its effect on the function of the renin-angiotensin system, which leads to fluid retention and increases uncontrolled hypertension.33,34 This finding highlights the urgency for interventions aimed at dietary salt restriction in patients with hypertension. Education on the recommended daily salt intake and limiting high-sodium foods epitomize such interventions.33,35
We discovered a high prevalence (38.5%) of medical comorbidities among our study participants and that they were highly associated with uncontrolled hypertension. Studies conducted in South Asia36 and China37 reflected a consistent finding where medical comorbidities, such as diabetes mellitus and chronic kidney disease, have been shown to increase the risk of uncontrolled hypertension. Extensive evidence has shown that controlling hypertension among hypertensive patients with chronic medical comorbidities might be challenging because many chronic medical diseases are secondary causes of hypertension.35–37 Considering the risk of engendering or aggravating hypertension in this population, the screening and early detection of hypertensive patients with medical comorbidities are salient in hypertension management.
It is well-known that lifelong compliance with AHMs is crucial in hypertension management.31,35 We observed that 42.1% of our study participants had poor compliance with AHMs. Our findings were slightly higher (6.5%) than the results of a systematic review that reported the pooled adherence to AHMs to be approximately 35.6% among LMICs.38 Additionally, consistent with existing literature, we noted that patients with poor compliance to AHMs had eight times higher odds of developing uncontrolled hypertension than those with good compliance to AHMs.35,38,39 The results of this study could evoke the development of effective drug adherence programs that may, in turn, help reduce uncontrolled hypertension and improve public health outcomes in Afghanistan and beyond.
The ongoing multidimensional conflict in Afghanistan and its inevitable psycho-social and economic consequences have undoubtedly contributed to the psychological problems of Afghans.40,41 The findings of this study portray a high prevalence (51.8%) of depressive symptoms in our study participants. Previous studies have shown that depression is common in patients with uncontrolled hypertension and may interfere with blood pressure control.33,42,43 Thus, screening and early detection of depression in hypertensive patients is a salient and cost-effective tool that may improve outcomes.43
Limitations
This study has several limitations. First, we measured blood pressure only at the follow-up visits instead of regular monitoring to determine blood pressure steady levels. Such glimpsed measurement may have engendered misclassification of some patients as either controlled or uncontrolled. Second, our data epitomize three public hospitals; therefore, making any generalization calls for caution. Third, the study overlooked specific factors such as patient education and secondary causes of hypertension, which may have impacted blood pressure control. Fourth, we employed the Pashtu versions of the PHQ-9 and the 14-item Hill-Bone compliance scales for the first time, while their psychometric properties require assertion. Finally, the cross-sectional design challenges the causal relationships between the variables. Therefore, we recommend future research with a longitudinal design that will flourish causal inferences between various variables.
Conclusion
The prevalence of uncontrolled hypertension was high (77.3%) in the present study. Physical inactivity, current smoking, high salt intake, medical comorbidity, higher BMI, poor compliance with AHMs, and depressive symptoms were associated with uncontrolled hypertension. These factors may epitomize potential targets for public/individual health interventions in Afghanistan and beyond.
Data Sharing Statement
The primary data used to support the findings of this study are available from the corresponding author upon request.
Ethical Approval
The Research and Ethics Committee (REC) of Kandahar University approved this study (Letter No. 83; Dated: 20/08/2022). Additionally, we followed the ethical principles outlined in the Declaration of Helsinki and the Good Clinical Practice (GCP) guidelines. The interviewer provided all potential participants with information concerning the study objectives, benefits/risks of participation, and the right to retract from the study at any time. Prior to their inclusion in the study, we obtained written informed consent from all participants.
Acknowledgments
We express our gratitude to the officials in Mirwais Regional Hospital, Ibni Sina Hospital, and Paktia provincial hospital. We offer special thanks to the subjects and data collectors of this study whose contribution made this study possible.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Nguyen TN, Chow CK. Global and national high blood pressure burden and control. Lancet. 2021;398(10304):932–933. doi:10.1016/s0140-6736(21)01688-3
2. Hedner T, Kjeldsen SE, Narkiewicz K. State of global health – hypertension burden and control. Blood Press. 2012;21(sup1):1–2. doi:10.3109/08037051.2012.704786
3. Sustainable Development Goals. Goal 3: ensure healthy lives and promote well-being for all at all ages. New York: United Nations; 2015. Available from: https://www.un.org/sustainabledevelopment/health.
4. Zhou B, Perel P, Mensah GA, Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol. 2021;18(11):785–802. doi:10.1038/s41569-021-00559-8
5. Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control. Circulation. 2016;134(6):441–450. doi:10.1161/circulationaha.115.018912
6. World Health Organization. Hypertension Afghanistan 2020 country profile; 2021. Available from: https://www.who.int/publications/m/item/hypertension-afg-country-profile-afghanistan-2020.
7. Saeed KMI. Burden of hypertension in the capital of Afghanistan: a cross-sectional study in Kabul City, 2015. Int J Hypertens. 2017;2017:1–7. doi:10.1155/2017/3483872
8. Lee CJ, Park WJ, Suh J, et al. Relationship between health‐related quality of life and blood pressure control in patients with uncontrolled hypertension. J Clin Hypertens. 2020;22(8):1415–1424. doi:10.1111/jch.13941
9. Adamu K, Feleke A, Muche A, et al. Health related quality of life among adult hypertensive patients on treatment in Dessie City, Northeast Ethiopia. PLoS One. 2022;17(9):e0268150. doi:10.1371/journal.pone.0268150
10. Sorato MM, Davari M, Kebriaeezadeh A, Sarrafzadegan N, Shibru T. Societal economic burden of hypertension at selected hospitals in southern Ethiopia: a patient-level analysis. BMJ Open. 2022;12(4):e056627. doi:10.1136/bmjopen-2021-056627
11. Wierzejska E, Giernaś B, Lipiak A, Karasiewicz M, Cofta M, Staszewski R. A global perspective on the costs of hypertension: a systematic review. Archiv Med Sci. 2020;16(5):1078–1091. doi:10.5114/aoms.2020.92689
12. World Health Organization. Afghanistan top 10 causes of death; 2020. Available from: https://www.worldlifeexpectancy.com/news/afghanistan-vs-pakistan-top-10-causes-of-death.
13. Rahimi BA, Hemat MD, Rahimy N, Rafiqi N, Kakar MAZ. Determinants of uncontrolled hypertension among hypertensive patients in Kandahar, Afghanistan. Online J Health Allied Sci. 2020;19(2):7.
14. Amare F, Hagos B, Sisay M, Molla B. Uncontrolled hypertension in Ethiopia: a systematic review and meta-analysis of institution-based observational studies. BMC Cardiovasc Disord. 2020;20(1). doi:10.1186/s12872-020-01414-3
15. Sisay Y, Abera H, Biratu TD, Legesse TG. Uncontrolled hypertension and behavioral risk factors among adult hypertensive patients at Saint Paul’s Hospital, Millennium Medical College, Addis Ababa, Ethiopia. Adv Public Health. 2022;16:1–7. doi:10.1155/2022/7518860
16. Nguyen HT, Hoang Thi Phuong N, Tran Nguyen N, Nguyen Anh T, Nguyen Dang V. Characterizing patients with uncontrolled blood pressure at an urban hospital in Hanoi, Vietnam. Int J Hypertens. 2020;10:1–7. doi:10.1155/2020/5710281
17. Koya SF, Pilakkadavath Z, Wilson T, et al. Population-level hypertension control rate in India: a systematic review and meta-analysis of community based non-interventional studies, 2001–2020. medRxiv. 2022. doi:10.1101/2022.04.09.22273638
18. Chobanian AV. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. JAMA. 2003;289(19):2560. doi:10.1001/jama.289.19.2560
19. Flack JM, Adekola B. Blood pressure and the new ACC/AHA hypertension guidelines. Trends Cardiovasc Med. 2020;30(3):160–164. doi:10.1016/j.tcm.2019.05.003
20. Riegel GR, Martins GB, Schmidt AG, et al. Self-reported adherence to physical activity recommendations compared to the IPAQ interview in patients with hypertension. Patient Prefer Adherence. 2019;13:209–214. doi:10.2147/ppa.s185519
21. Hallal PC, Victora CG. Reliability and validity of the International Physical Activity Questionnaire (IPAQ). Med Sci Sports Exerc. 2004;36(3):556. doi:10.1249/01.mss.0000117161.66394.07
22. Kim MT, Hill MN, Bone LR, Levine DM. Development and testing of the hill-bone compliance to high blood pressure therapy scale. Prog Cardiovasc Nurs. 2000;15(3):906. doi:10.1111/j.1751-7117.2000.tb00211.x
23. Song Y, Han H-R, Song H-J, Nam S, Nguyen T, Kim MT. Psychometric evaluation of hill-bone medication adherence subscale. Asian Nurs Res. 2011;5(3):183–188. doi:10.1016/j.anr.2011.09.007
24. Chia YC, Devaraj NK, Ching SM, et al. Relationship of an adherence score with blood pressure control status among patients with hypertension and their determinants: findings from a nationwide blood pressure screening program. J Clin Hypertens. 2021;23(3):638–645. doi:10.1111/jch.14212
25. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9. J Gen Intern Med. 2001;16(9):606–613. doi:10.1046/j.1525-1497.2001.016009606.x
26. Bhana A, Rathod SD, Selohilwe O, Kathree T, Petersen I. The validity of the Patient Health Questionnaire for screening depression in chronic care patients in primary health care in South Africa. BMC Psychiatry. 2015;15(1). doi:10.1186/s12888-015-0503-0
27. International Business Machines Corporation. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY, USA: IBM Corporation; 2012.
28. Saasita PK, Senoga S, Muhongya K, Agaba DC, Migisha R. High prevalence of uncontrolled hypertension among patients with type 2 diabetes mellitus: a hospital-based cross-sectional study in southwestern Uganda. Pan African Med J. 2021;39. doi:10.11604/pamj.2021.39.142.28620
29. Steffen PR, Sherwood A, Gullette ECD, Georgiades A, Hinderliter A, Blumenthal JA. Effects of exercise and weight loss on blood pressure during daily life. Med Sci Sports Exerc. 2001;33(10):1635–1640. doi:10.1097/00005768-200110000-00004
30. Harsha DW, Bray GA. Weight loss and blood pressure control (Pro). Hypertension. 2008;51(6):1420–1425. doi:10.1161/hypertensionaha.107.094011
31. Kjeldsen SE, Hedner T, Jamerson K, et al. Hypertension Optimal Treatment (HOT) study. Hypertension. 1998;31(4):1014–1020. doi:10.1161/01.hyp.31.4.1014
32. Goel S, Singh H, Sharma S, Kathiresan J, Bhatt G. Tobacco use and uncontrolled hypertension among Indian men: insights from the National Family Health Survey (NFHS-4), 2015–2016. J Fam Med Prim Care. 2022;11(9):5792. doi:10.4103/jfmpc.jfmpc_163_22
33. De Keyzer W, Tilleman K, Ampe J, De Henauw S, Huybrechts I. Effect of sodium restriction on blood pressure of unstable or uncontrolled hypertensive patients in primary care. Nutr Res Pract. 2015;9(2):180. doi:10.4162/nrp.2015.9.2.180
34. Khamidullaeva G, Khafisova L, Nagay A, Kurbanova D, Srojidinova N. THE ROLE OF HIGH DIETARY SALT INTAKE IN DEVELOPMENT OF RESISTANT HYPERTENSION. J Hypertens. 2018;36(Supplement 1):e53. doi:10.1097/01.hjh.0000539108.88656.fa
35. Gebremichael GB, Berhe KK, Zemichael TM. Uncontrolled hypertension and associated factors among adult hypertensive patients in Ayder comprehensive specialized hospital, Tigray, Ethiopia, 2018. BMC Cardiovasc Disord. 2019;19(1). doi:10.1186/s12872-019-1091-6
36. Jafar TH, Gandhi M, Jehan I, et al. Determinants of uncontrolled hypertension in rural communities in South Asia—Bangladesh, Pakistan, and Sri Lanka. Am J Hypertens. 2018;31(11):1205–1214. doi:10.1093/ajh/hpy071
37. Yang L, Xu X, Yan J, et al. Analysis on associated factors of uncontrolled hypertension among elderly hypertensive patients in Southern China: a community-based, cross-sectional survey. BMC Public Health. 2014;14(1). doi:10.1186/1471-2458-14-903
38. Nielsen JØ, Shrestha AD, Neupane D, Kallestrup P. Non-adherence to anti-hypertensive medication in low- and middle-income countries: a systematic review and meta-analysis of 92443 subjects. J Hum Hypertens. 2016;31(1):14–21. doi:10.1038/jhh.2016.31
39. Sarfo FS, Mobula LM, Burnham G, et al. Factors associated with uncontrolled blood pressure among Ghanaians: evidence from a multicenter hospital-based study. PLoS One. 2018;13(3):e0193494. doi:10.1371/journal.pone.0193494
40. Kovess-Masfety V, Keyes K, Karam E, Sabawoon A, Sarwari BA. A national survey on depressive and anxiety disorders in Afghanistan: a highly traumatized population. BMC Psychiatry. 2021;21(1). doi:10.1186/s12888-021-03273-4
41. Rahimi MP, Wafa MH, Stanikzai MH, Rahimi BA. Post-traumatic stress disorder (PTSD) probability among parents who live in Kandahar, Afghanistan and lost at least a child to armed conflict. Sci Rep. 2023;13(1). doi:10.1038/s41598-023-31228-0
42. Abreu-Silva E, Todeschini A. Depression and its relation with uncontrolled hypertension and increased cardiovascular risk. Curr Hypertens Rev. 2014;10(1):8–13. doi:10.2174/157340211001141111144533
43. Hamrah MS, Hamrah MH, Ishii H, et al. Anxiety and depression among hypertensive outpatients in Afghanistan: a cross-sectional study in Andkhoy City. Int J Hypertens. 2018;2018:1–8. doi:10.1155/2018/8560835
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
