Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 16
Optimizing Type 2 Diabetes Management in a Medically Complex Patient: A Case Report of a Patient with Type 2 Diabetes and HIV
Authors Kabakambira JD , Kong JM
Received 8 May 2023
Accepted for publication 5 August 2023
Published 11 August 2023 Volume 2023:16 Pages 2401—2406
DOI https://doi.org/10.2147/DMSO.S415949
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Juei-Tang Cheng
Jean Damascene Kabakambira,1 Jason M Kong2
1Department of Medicine, University of Rwanda, Kigali, Rwanda; 2Division of Endocrinology, University of British Columbia, Vancouver, BC, Canada
Correspondence: Jean Damascene Kabakambira, Department of Medicine, University of Rwanda, KN 4th Avenue, P.O Box 655, Kigali, Rwanda, Tel +250788800966, Email [email protected]
Background: The prevalence of diabetes is rapidly escalating, with projections indicating that 783 million individuals aged 20– 79 years worldwide will be affected by diabetes. This rise is concurrent with a persistent prevalence of HIV in developing nations, while conventional risk factors such as sedentary lifestyle and unhealthy diet may account for this trend, HIV and its treatment have emerged as potential contributing factors. Achieving optimal diabetes control in patients with HIV necessitates a profound understanding of the intricate interplay between the two diseases and their respective treatments.
Case Report: We present a case involving a patient with long standing type 2 diabetes, coexisting HIV infection and hypertension. Despite receiving high doses of insulin, as advised by most diabetes guidelines, the patient’s diabetes remained poorly controlled. In lieu of strictly adhering to guidelines, our primary focus was to conduct a comprehensive reevaluation of the patient’s medications, prioritizing the development of streamlined and safe treatment regimens for all three of her medical conditions. Employing this strategy, we observed swift improvement in blood glucose levels, leading to successful diabetes control within one year.
Conclusion: This case underscores the importance of individualizing diabetes management in patients with multiple comorbidities. It highlights the significance of reassessing treatment approaches beyond standard guidelines, with a focus on tailoring therapy to suit the unique needs and complexities of each patient’s medical profile. Such personalized interventions hold promise for achieving optimal diabetes control in individuals with diverse comorbidities.
Keywords: diabetes, HIV, case report, Rwanda
Introduction
The burden of type 2 diabetes is alarmingly increasing across the world. In Africa, where HIV infection is still significantly prevalent, it can be quite challenging to improve glycemic control in patients with the two diseases due to multiple factors. Additionally, the association of diabetes and HIV infection confers an increased risk of macrovascular and microvascular complications. This case report highlights the importance of individualized treatment plans that consider the unique needs of patients with multiple chronic conditions.
It shows the steps taken and the rationale of interventions that led to optimal diabetes control after a period of 12 months.
Case Presentation
A 59-year-old woman presented to our Diabetes Clinic in August 2020 at the University Teaching Hospital of Kigali, Rwanda. Her chief complaint was the persistent high blood sugar despite being on insulin therapy. She carried three diagnoses – type 2 diabetes, hypertension and Human Immunodeficiency Virus (HIV) infection, all diagnosed 20 years earlier.
She was treated with mixed insulin 36 UI twice a day, Telmisartan-Hydrochlorothiazide 40/12.5 mg once daily, aspirin 75mg once daily, and a combination of dolutegravir, abacavir, and lamivudine. Her blood sugar was always above 180 mg/dl with frequent readings around 300 mg/dl.
Her physical exam was consistent with elevated blood pressure (141/99 mmHg) and obesity (body mass index: 33.7 kg/m2, waist circumference: 115 cm). Her laboratory work-up on arrival showed a HbA1C of 12.1% with a random plasma glucose of 14.9 mmol/L, and a C-peptide level of 513 pmol/L, which suggested preserved pancreatic beta islet cell function. She had kidney derangement (GFR of 50 mL/min with no evidence of microalbuminuria) and dyslipidemia (Table 1).
 |
Table 1 Baseline and Follow Up Laboratory Findings at 6 and 12 Months |
Management and Outcome
The patient was counseled on the importance of dietary and lifestyle modifications. Although most guidelines recommend using insulin in patients with poorly controlled diabetes, the patient had had poor glycemic control despite being on insulin for more than 10 years. Her insulin was therefore discontinued and switched to oral antidiabetic medications (Vildagliptin/Metformin 50/500 mg twice daily and Gliclazide modified release 120 mg once daily). Her blood pressure medications were revised to remove hydrochlorothiazide and optimize telmisartan, while dolutegravir was substituted for efavirenz in her antiretroviral therapy regimen. Finally, she was commenced on statin therapy for hypercholesterolemia. The patient achieved diabetes control after 12 months of new interventions while experiencing tremendous improvement in other metabolic parameters (Table 1, Figures 1 and 2).
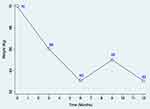 |
Figure 1 Body weight trend over one year of follow-up. |
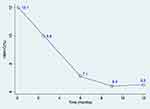 |
Figure 2 HBA1C trend over one year of follow-up. |
Discussion
Insulin Therapy: A Life Sentence?
For so long, insulin has been the mainstay treatment for refractory poor glycemic control. Several guidelines recommend the use of insulin or several oral antidiabetic drugs in patients with poor glycemic control.1 There are many factors associated with poor glycemic control despite using insulin, the last resort in type 2 diabetes treatment.
Complexity of Insulin Use
Since its discovery a century ago, injectable insulin analogues remain the only effective route for insulin administration and can require up to 4 or more injections in a day. Individuals may have difficulty accurately measuring and administering the correct dose. In some cases, patients may also experience injection site reactions, which can be painful and uncomfortable.
Furthermore, blood glucose levels can vary significantly throughout the day and can be influenced by factors such as diet, physical activity and stress. Insulin dosing needs to be adjusted accordingly to maintain stable blood glucose levels. Frequent blood glucose monitoring, in addition to regular multiple daily insulin injections, can bring the total needle sticks to more than 10 in a single day which can be too burdensome. Recent technologies such as continuous glucose monitoring are widely unavailable even in developed countries. Even the traditional tools of blood glucose monitoring (glucometers, strips and needles) and insulin itself are still unaffordable in many parts of the world. A study by Klatman et al looking at the cost of insulin and monitoring of blood glucose tool kits revealed a wide gap compared to the GDP in low-income and middle-income countries2 (Figure 3). Our patient confided that she sometimes injected insulin without checking her blood sugar. In fact, the maximum allowed blood glucose testing kits were not enough to cover the entire period required before she could get a refill.
 |
Figure 3 Direct costs of insulin and self-monitoring of blood glucose for families in low-income and middle-income countries.2 Abbreviation: SMBG, self-monitoring of blood glucose. Notes: Data are from the World Health Organization (WHO Diabetes Country Profiles 2016) and are the typical supply costs for a family with one child with type 1 diabetes. *The amount of insulin required was assumed to be 18 vials of 100 IU/mL human insulin (or equivalent volume of 40 IU/mL). †Government provides insulin for free. ‡Cost updated from previous data. |
Determinants of Insulin Efficacy
It is important to note that insulin therapy may not always lead to optimal diabetes control. While insulin is a critical component of diabetes management, it is only one piece of the puzzle. Diabetes management also involves lifestyle changes, such as dietary modifications and increase in physical activity, as well as regular monitoring of blood sugar levels and other health parameters. Failure to address all aspects of diabetes management can result in poor diabetes control, even with insulin therapy.
Additionally, insulin preservation requires special conditions such as cool temperature. Many users may not have access to refrigerators which will have an impact on insulin quality.
Our patient was a public servant who worked from a shared office. She had no access to prepare her meals or heat her packed lunch. She therefore grabbed whatever available pastries for lunch. Additionally, there was no refrigerator to conserve insulin. Consequently, she was unable to bolus insulin for her carbohydrate-rich lunches.
All these factors contributed to sub-optimal use of insulin in terms of frequency and dosing adequacy which potentially explained the long-standing poor diabetes control.
Despite being on insulin, her blood glucose records were persistently above her target goals. She still had relatively good pancreatic beta cell mass which gave us confidence to trial her on oral antidiabetic medications while discontinuing insulin.
Perpetuation of Insulin Resistance
Insulin therapy often leads to weight gain, which can worsen insulin resistance. In some cases, excessive weight gain may contribute to higher morbidity and mortality rates if this leads to patient resistance to intensifying insulin therapy. Insulin-induced weight gain may occur due to a variety of factors, including the anabolic properties of insulin, the fear or experience of hypoglycemia leading to defensive snacking, and the quasi-physiological subcutaneous insulin absorption. Strategies for limiting insulin-associated weight gain include improving insulin sensitivity through changes in diet, exercise, or medications that enhance insulin sensitivity. Efforts to replace insulin using regimens that more closely replicate the body’s natural processes should also enable more efficient dosing of insulin.3
Blood Pressure Medication and Insulin Resistance
Thiazides are notoriously known to cause insulin resistance. A study comparing hydrochlorothiazide to candesartan and placebo revealed that hydrochlorothiazide increased visceral fat, liver fat and insulin resistance after only 12 weeks of use.4 A meta-analysis looking at clinical trials using diuretics from 1966 to 2004 established a causal relationship between the use of thiazides, hypokalemia and rise in glucose.5 Although the exact mechanism has not been elucidated for thiazide-induced glucose intolerance, one theory suggests that the relationship between thiazide-induced hypokalemia and insulin secretion is part of the mechanism.6 For this reason, hydrochlorothiazide was discontinued in our patient, and angiotensin receptor blocker was optimized to maintain normal blood pressure. The patient also experienced improvement of the kidney function after 6 months following these changes.
Antiretroviral Therapy and Insulin Resistance
Integrase strand transfer inhibitors (INSTIs) are increasingly used in patients living with HIV due to their safety, effectiveness and high genetic barrier. In Rwanda, the 2018 HIV guideline recommends initiating adolescent and adult patients on INSTI (dolutegravir) at the expense of efavirenz with the exception of pre-menopausal women.7 Later on, this new molecule was escalated to the general population as part of first-line therapy.
Unfortunately, there is accumulating evidence that INSTIs are associated with insulin resistance. The exact mechanisms underlying the diabetogenic effects of INSTIs are not yet fully understood, but current evidence suggests that INSTIs may induce beta-cell dysfunction and apoptosis, reduce insulin secretion, ultimately leading to impaired glucose metabolism.8
Additionally, INSTIs may interfere with glucose homeostasis by affecting insulin signaling pathways, leading to impaired glucose tolerance and insulin resistance. INSTIs may also lead to changes in body composition, including increased visceral adipose tissue, which is associated with an increased risk of insulin resistance and metabolic dysfunction.9 We believe that substituting efavirenz for dolutegravir in our patient’s antiretroviral therapy played a crucial role in getting her diabetes under control quickly.
Conclusions
This case report presents a patient with type 2 diabetes, HIV and hypertension who achieved diabetes control by substituting insulin with cheaper oral antidiabetic medications, which deviates from conventional guidelines. This highlights the importance of individualizing diabetes drug therapy and recognizing potential drug interactions in the management of complex patients with diabetes and multiple commodities.
Ethical Approval
The concerned patient provided a written consent for publication of their de-identified clinical information. The hospital’s ethical review board granted permission to publish this information.
Funding
The study was not funded.
Disclosure
The authors declare no competing interest in this work.
References
1. ElSayed NA, Aleppo G, Aroda VR, et al. 9. Pharmacologic approaches to glycemic treatment: standards of care in diabetes—2023. Diabetes Care. 2023;46(Supplement_1):S140–S157. doi:10.2337/dc23-S009
2. Klatman EL, Jenkins AJ, Ahmedani MY, Ogle GD. Blood glucose meters and test strips: global market and challenges to access in low-resource settings. Lancet Diabetes Endocrinol. 2019;7(2):150–160. doi:10.1016/S2213-8587(18)30074-3
3. Samuel VT, Shulman GI. The pathogenesis of insulin resistance: integrating signaling pathways and substrate flux. J Clin Invest. 2016;126(1):12–22. doi:10.1172/JCI77812
4. Eriksson JW, Jansson PA, Carlberg B, et al. Hydrochlorothiazide, but not candesartan, aggravates insulin resistance and causes visceral and hepatic fat accumulation: the mechanisms for the diabetes preventing effect of Candesartan (MEDICA) Study. Hypertension. 2008;52(6):1030–1037. doi:10.1161/HYPERTENSIONAHA.108.119404
5. Zillich AJ, Garg J, Basu S, Bakris GL, Carter BL. Thiazide diuretics, potassium, and the development of diabetes: a quantitative review. Hypertension. 2006;48(2):219–224. doi:10.1161/01.HYP.0000231552.10054.aa
6. Houston MC. The effects of antihypertensive drugs on glucose intolerance in hypertensive nondiabetics and diabetics. Am Heart J. 1988;115(3):640–656. doi:10.1016/0002-8703(88)90816-2
7. RBC. HIV guideline 2018 Rwanda - google search. Available from: https://www.google.com/search?q=RBC+HIV+guideline+2018+Rwanda&sxsrf=AJOqlzW4DMen9ADBauoJoy7WHbVPSlwIaw%3A1678644200693&ei=6BMOZOX7KZvl0PEPnoW00Ao&ved=0ahUKEwjlj6X6_Nb9AhWbMjQIHZ4CDaoQ4dUDCA8&uact=5&oq=RBC+HIV+guideline+2018+Rwanda&gs_lcp=Cgxnd3Mtd2l6LXNlcnAQAzIFCAAQogQyBQgAEKIEMgUIABCiBDIHCAAQHhCiBDoKCAAQRxDWBBCwAzoECCMQJ0oECEEYAFDABFjzE2DNF2gBcAF4AIABdogBgQOSAQM0LjGYAQCgAQHIAQjAAQE&sclient=gws-wiz-serp.
8. Fong PS, Flynn DM, Evans CD, Korthuis PT. Integrase strand transfer inhibitor-associated diabetes mellitus: a case report. Int J STD AIDS. 2017;28(6):626–628. doi:10.1177/0956462416675107
9. O’Halloran JA, Sahrmann J, Parra-Rodriguez L, et al. Integrase strand transfer inhibitors are associated with incident diabetes mellitus in people with human immunodeficiency virus. Clin Infect Dis. 2022;75(12):2060–2065. doi:10.1093/cid/ciac355
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
